- Home
- About Journals
-
Information for Authors/ReviewersEditorial Policies
Publication Fee
Publication Cycle - Process Flowchart
Online Manuscript Submission and Tracking System
Publishing Ethics and Rectitude
Authorship
Author Benefits
Reviewer Guidelines
Guest Editor Guidelines
Peer Review Workflow
Quick Track Option
Copyediting Services
Bentham Open Membership
Bentham Open Advisory Board
Archiving Policies
Fabricating and Stating False Information
Post Publication Discussions and Corrections
Editorial Management
Advertise With Us
Funding Agencies
Rate List
Kudos
General FAQs
Special Fee Waivers and Discounts
- Contact
- Help
- About Us
- Search

The Open Family Studies Journal
(Discontinued)
ISSN: 1874-9224 ― Volume 12, 2020
The Edinburgh Postnatal Depression Scale: Model Comparison of Factor Structure and its Psychosocial Correlates Among Mothers at One Month After Childbirth in Japan
Ayako Hada1, 2, 3, *, Chika Kubota4, 8, Masumi Imura3, Fumie Takauma5, Katsuhiko Tada6, Toshinori Kitamura1, 2, 7, 8
Abstract
Background:
The Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden & Sagovsky, 1987) has been widely used as a screening instrument. It is also used as a measure of Postnatal Depression (PND) severity. Various EPDS factor structure models have been proposed in many studies without an unequivocal conclusion. We compared first-order, higher-order factor, and bifactor models of the EPDS, and examined possible predictors of subscales by Structural Equation Modelling (SEM).
Methods:
Data came from a follow-up study of 758 women after childbirth on two occasions (five days and one month postnatal). We used the EPDS together with items tapping Negative Life Events (NLEs) and coping styles and behaviours.
Results:
The bifactor model showed the best fit with data compared with all other models: CFI = 0.999, RMSEA = 0.14, and AIC = 79.637. A single general dimension alongside three distinct subfactors (anhedonia, anxiety, and dysphoria) was predicted differentially by various predictor variables.
Conclusion:
Our study expanded on a previous factor structural study of the EPDS and developed the hierarchical (bifactor) model. The model’s construct validity was confirmed by its meaningful associations with NLEs and coping styles and behaviours.
Article Information
Identifiers and Pagination:
Year: 2019Volume: 11
First Page: 1
Last Page: 17
Publisher Id: TOFAMSJ-11-1
DOI: 10.2174/1874922401911010001
Article History:
Received Date: 02/03/2019Revision Received Date: 09/04/2019
Acceptance Date: 22/04/2019
Electronic publication date: 31/05/2019
Collection year: 2019
open-access license: This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International Public License (CC-BY 4.0), a copy of which is available at: https://creativecommons.org/licenses/by/4.0/legalcode. This license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
* Address correspondence to this author at the Kitamura Institute of Mental Health Tokyo, Flat A, 2-26-3, Tomigaya, Shibuya, Tokyo, Japan;
Tel: +81-03-5738-8371; E-mail: ayako-ha.fbm@jcom.zaq.ne.jp
| Open Peer Review Details | |||
|---|---|---|---|
| Manuscript submitted on 02-03-2019 |
Original Manuscript | The Edinburgh Postnatal Depression Scale: Model Comparison of Factor Structure and its Psychosocial Correlates Among Mothers at One Month After Childbirth in Japan | |
1. INTRODUCTION
Postnatal depression (PND) is a depressive disorder for which onset is within one month after childbirth [1American Psychiatric Association. Diagnostic and statistical manual of mental disorders 5th ed. 2013.]. Its prevalence is approximately 13% [2Beck CT. Predictors of postpartum depression: An update. Nurs Res 2001; 50(5): 275-85.
[http://dx.doi.org/10.1097/00006199-200109000-00004] [PMID: 115 70712] , 3O’hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. Int Rev Psychiatry 1996; 8(1): 37-54.
[http://dx.doi.org/10.3109/09540269609037816] ] worldwide and, in Japan, it is approximately 5% [4Kitamura T, Yoshida K, Okano T, et al. Multicentre prospective study of perinatal depression in Japan: Incidence and correlates of antenatal and postnatal depression. Arch Women Ment Health 2006; 9(3): 121-30.
[http://dx.doi.org/10.1007/s00737-006-0122-3] [PMID: 16547826] ]. PND is a mental health issue for both women and their children. For example, the prevalence of perinatal women who have thoughts of self-harm is 5–14%, and the prevalence of suicides as the cause of women’s death within one year after childbirth reaches 20% [5Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Women Ment Health 2005; 8(2): 77-87 .
[http://dx.doi.org/10.1007/s00737-005-0080-1] ]. PND also has negative effects on early mother-infant relationships and child development [6Moehler E, Brunner R, Wiebel A, Reck C, Resch F. Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother-child bonding. Arch Women Ment Health 2006; 9(5): 273-8.
[http://dx.doi.org/10.1007/s00737-006-0149-5] [PMID: 16937313] , 7Wan MW, Green J. The impact of maternal psychopathology on child-mother attachment. Arch Women Ment Health 2009; 12(3): 123-34.
[http://dx.doi.org/10.1007/s00737-009-0066-5] ]. The child-caring ability of mothers with PND is impaired [8Leiferman JA, Ollendick TH, Kunkel D, et al. Mothers' mental distress and parenting practices with infants and toddlers. Arch Women Ment Health 2005; 8(4): 243-47.-10Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics 2006; 118(2): 659-68.
[http://dx.doi.org/10.1542/peds.2005-2948] [PMID: 16882821] ]. Thus, PND is a major health issue for families.
As a means of PND screening, many instruments have been developed [11Boyd RC, Le HN, Somberg R. Review of screening instruments for postpartum depression. Arch Women Ment Health 2005; 8(3): 141-53.
[http://dx.doi.org/10.1007/s00737-005-0096-6] [PMID: 16133785] , 12Brodey BB, Goodman SH, Baldasaro RE, et al. Development of the Perinatal Depression Inventory (PDI)-14 using item response theory: a comparison of the BDI-II, EPDS, PDI, and PHQ-9. Arch Women Ment Health 2016; 19(2): 307-16.
[http://dx.doi.org/10.1007/s00737-015-0553-9] [PMID: 26271280] ] Among them is the Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden & Sagovsky, 1987) [13Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987; 150(6): 782-6.
[http://dx.doi.org/10.1192/bjp.150.6.782] [PMID: 3651732] ], which was translated into multiple languages and evaluated in many countries including Japan [14Okano T, Murata M, Masuji F, et al. Validation and reliability of Japanese version of the EPDS. Arch Psychiatr Diagn Clin Evaluation 1996; 74: 525-33. [in Japanese].]. Although the EPDS was developed as a screening instrument with a cut-off point to identify women who are likely to suffer from PND, it has also been used as a measure of PND severity [15Chen C, Gao J, Zhang J, Jia L, Yu T, Zheng Y. Serum leptin level measured 48 h after delivery is associated with development of postpartum depressive symptoms: A 3-month follow-up study. Arch Women Ment Health 2016; 19(6): 1001-8.
[http://dx.doi.org/10.1007/s00737-016-0647-z] [PMID: 27295066] -19Takehara K, Tachibana Y, Yoshida K, Mori R, Kakee N, Kubo T. Prevalence trends of pre- and postnatal depression in Japanese women: A population-based longitudinal study. J Affect Disord 2018; 225: 389-94.
[http://dx.doi.org/10.1016/j.jad.2017.08.008] [PMID: 28846961] ].
Similar to other types of depression, the symptomatology of PND is multifaceted. The number of factors of PND symptomatology differs from one to three in previous studies. Thus, configural invariance remains debatable. For example, a Norwegian study of the EPDS [20Berle JØ, Aarre TF, Mykletun A, Dahl AA, Holsten F. Screening for postnatal depression. Validation of the Norwegian version of the Edinburgh Postnatal Depression Scale, and assessment of risk factors for postnatal depression. J Affect Disord 2003; 76(1-3): 151-6.
[http://dx.doi.org/10.1016/S0165-0327(02)00082-4] [PMID: 12943 945] ] was reported to have a single-component structure by Principal Component Analysis (PCA) in a sample of 411 women at six to 12 weeks postpartum. The French version of the EPDS was also examined by PCA, and a two-component structure was detected in a sample of 87 women in the first four months postpartum [21Guedeney N, Fermanian J. Validation study of the French version of the Edinburgh Postnatal Depression Scale (EPDS): New results about use and psychometric properties. Eur Psychiatry 1998; 13(2): 83-9.
[http://dx.doi.org/10.1016/S0924-9338(98)80023-0] [PMID: 19698 604] ]. Tuohy et al. [22Tuohy A, McVey C. Subscales measuring symptoms of non-specific depression, anhedonia, and anxiety in the Edinburgh Postnatal Depression Scale. Br J Clin Psychol 2008; 47(Pt 2): 153-69.
[http://dx.doi.org/10.1111/j.2044-8260.2008.tb00463.x] [PMID: 177 61026] ], in a PCA study, reported that the English version of the EPDS had a three-component structure including anhedonia, anxiety, and depression. Similarly, the Vietnamese, Turkish, and Filipino versions of the scale by PCA at six to nine months postpartum were examined and it was reported that these versions of the EPDS had a three-component structure [23Small R, Lumley J, Yelland J, Brown S. The performance of the Edinburgh Postnatal Depression Scale in English speaking and non-English speaking populations in Australia. Soc Psychiatry Psychiatr Epidemiol 2007; 42(1): 70-8.
[http://dx.doi.org/10.1007/s00127-006-0134-3] [PMID: 17102922] ]. Previously, PCAs and EFAs that were statistically different [24Yong AG, Pearce S. A beginner’s guide to factor analysis: Focusing on exploratory factor analysis. Tutor Quant Methods Psychol 2013; 9(2): 79-94.
[http://dx.doi.org/10.20982/tqmp.09.2.p079] ] were not distinguished and were treated as if they were interchangeable [25Ross LE, Gilbert Evans SE, Sellers EM, Romach MK. Measurement issues in postpartum depression part 1: Anxiety as a feature of postpartum depression. Arch Women Ment Health 2003; 6(1): 51-7.]. EFAs are preferable to PCAs because PCAs are the only data reduction method without regard to any underlying structure caused by latent variables [26Costello AB, Osborne JW. Best practices in explanatory factor analysis: Four recommendations for getting the most from your analysis. Pract Assess, Res Eval 2005; 10(7): 1-9.]. The component calculation is based on using all the variance of the indicators. This is in contrast to the idea of EFAs where researchers analyse data with a Priori theory of internal structures.
Many studies reported that the EPDS had a three-factor structure. Kubota et al. [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ], in a sample of 690 women at one-month postpartum, used the Japanese version of the EPDS where three factors emerged: anhedonia, anxiety, and depression. Takehara et al. [19Takehara K, Tachibana Y, Yoshida K, Mori R, Kakee N, Kubo T. Prevalence trends of pre- and postnatal depression in Japanese women: A population-based longitudinal study. J Affect Disord 2018; 225: 389-94.
[http://dx.doi.org/10.1016/j.jad.2017.08.008] [PMID: 28846961] ] re-examined the three-factor structure of the Japanese version of the EPDS reported by Kubota et al. [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ]. This was a six-time-point study from pregnancy to postpartum in a sample of 1,311 women in Japan. The same three-factor structure was confirmed.
A drawback of EFAs is the choice of the number of factors that are subjectively defined by the researchers. This results in different models of the factor structure. To identify the best factor structure of the EPDS, Confirmatory Factor Analysis (CFA) is necessary.
The model fit of the past investigations of the EPDS CFA studies is presented in Table 1. The Comparative Fit Index (CFI) ranged from 0.93 to 0.999 and was less than 0.97 approximately half the time. The Root Mean Square Error of Approximation (RMSEA) ranged from 0.00 to 0.10 and it was greater than 0.05 approximately 60% of the time. Therefore, the fit of the factor structure model of the EPDS among the past studies was only modest.
This may mean that a simple first-order one-factor model of the EPDS factor structure did not necessarily represent the real picture of the item structure. Little has been argued regarding whether a higher order (or hierarchical) structure of PND exists. For example, in addition to subscales of PND including anhedonia, anxiety, and depression, we may expect a general factor of PND severity. This echoes the general factor of intelligence [28Brunner M, Nagy G, Wilhelm O. A tutorial on hierarchically structured constructs. J Pers 2012; 80(4): 796-846.
[http://dx.doi.org/10.1111/j.1467-6494.2011.00749.x] [PMID: 2209 1867] ].
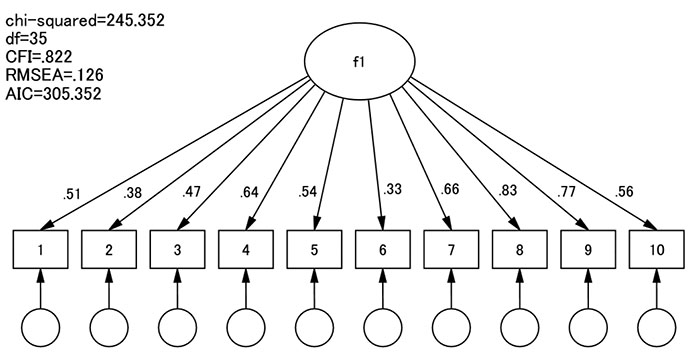
In EFAs, the number of factors ranges between one and the number of items of the instrument. Thus, in the EPDS that consisted of 10 items, the number of factors in EFAs could range between one and 10. We compare in CFAs different factor structure models derived from EFAs. A single-factor model is the most parsimonious model (Fig. 1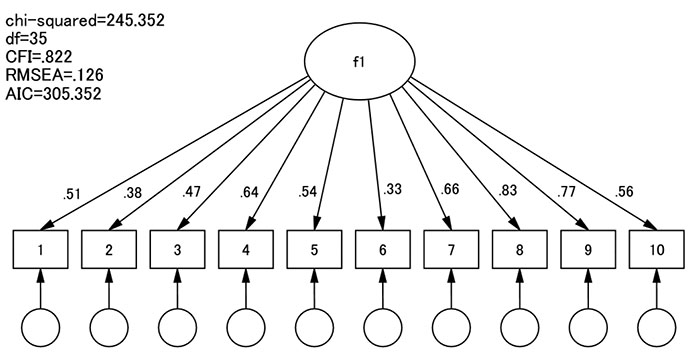 ). This model predicts that individual differences in all the EPDS items are caused by individual differences in only one common latent factor. The influence of this general factor is represented by a factor loading that is depicted in the figure as a single-headed arrow. A single factor model has the greatest number of df. When the single-factor model does not fit the data satisfactorily, we should consider a first-order factor model with more than one latent factor; for example, a two-factor model. In this model, each EPDS item is considered to be influenced by one of the first-order factors (Figs. 2
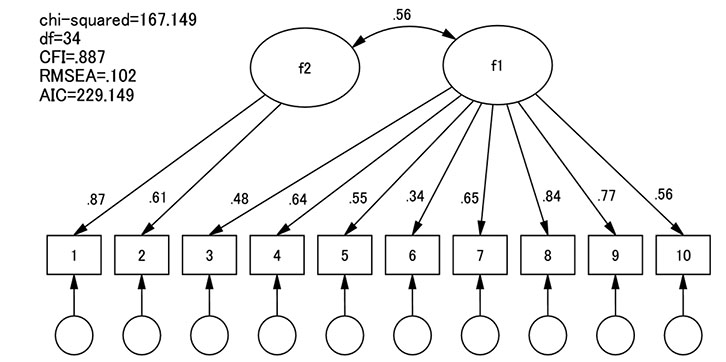
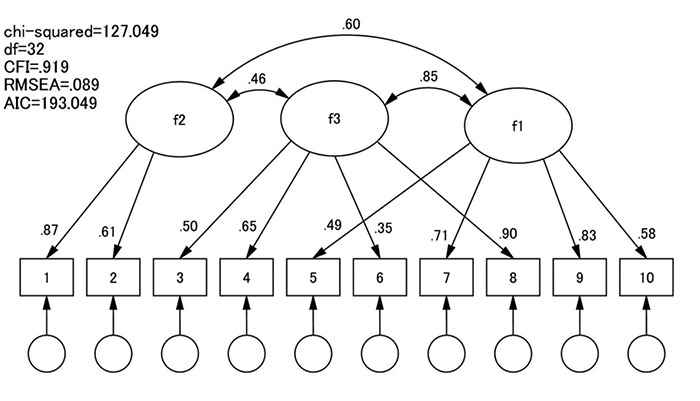
). This model predicts that individual differences in all the EPDS items are caused by individual differences in only one common latent factor. The influence of this general factor is represented by a factor loading that is depicted in the figure as a single-headed arrow. A single factor model has the greatest number of df. When the single-factor model does not fit the data satisfactorily, we should consider a first-order factor model with more than one latent factor; for example, a two-factor model. In this model, each EPDS item is considered to be influenced by one of the first-order factors (Figs. 2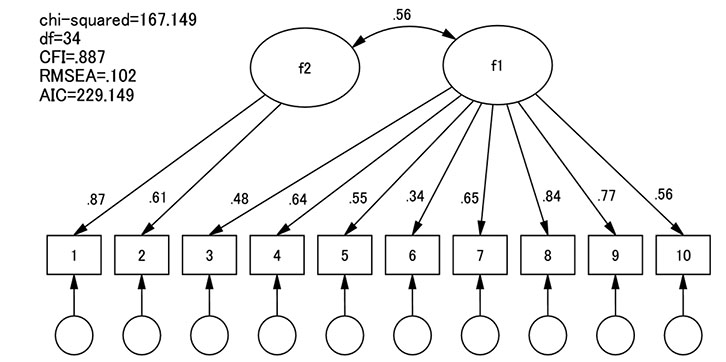 and 3
and 3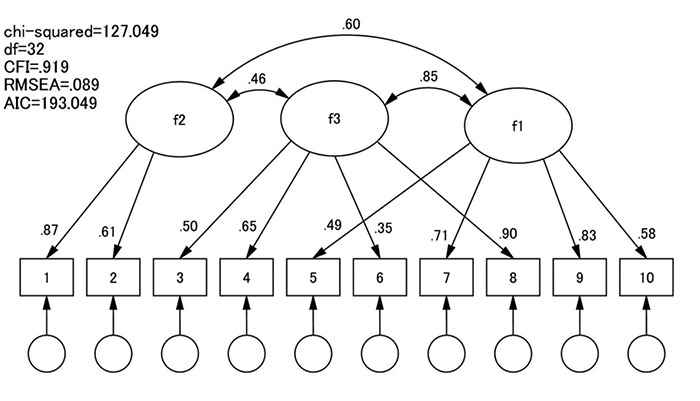 ). In a two-factor model of the EPDS, for example, items 1 and 2 are influenced only by the second factor, whereas the other eight items are influenced only by the first factor. The first-order factors are considered to be correlated with each other. If all the factor correlations in a first-factor model are fixed to r =1.0, it is equivalent to the single-factor model. Therefore, the former nests the latter. The df of a first-order factor model is lower than that of a single-factor model. If χ2 decreases significantly for the df difference, we adopt the first-order model,whereas if χ2 does not decrease significantly for the df difference between the two models, we retain the single-factor model as the best model for the sake of parsimony. This procedure will be continued to a model with a greater number of factors until the χ2 difference does not reach the significance level.
). In a two-factor model of the EPDS, for example, items 1 and 2 are influenced only by the second factor, whereas the other eight items are influenced only by the first factor. The first-order factors are considered to be correlated with each other. If all the factor correlations in a first-factor model are fixed to r =1.0, it is equivalent to the single-factor model. Therefore, the former nests the latter. The df of a first-order factor model is lower than that of a single-factor model. If χ2 decreases significantly for the df difference, we adopt the first-order model,whereas if χ2 does not decrease significantly for the df difference between the two models, we retain the single-factor model as the best model for the sake of parsimony. This procedure will be continued to a model with a greater number of factors until the χ2 difference does not reach the significance level.
The difference between single- and first-order factor models lies in the fact that the former focuses on general abilities (e.g., severity of depression), whereas the latter focuses on several specific abilities (e.g., anhedonia, anxiety, and dysphoria among depression symptoms). We consider that the general and specific abilities are located at different levels of the ability hierarchy. Neither model addresses both general and specific abilities simultaneously. When, as is the case of many psychological measurements, the models of a single- or first-factor structure do not satisfactorily fit the data, it is plausible to consider higher-order factor and bifactor models. These models take into account the general and specific abilities in their entirety [28Brunner M, Nagy G, Wilhelm O. A tutorial on hierarchically structured constructs. J Pers 2012; 80(4): 796-846.
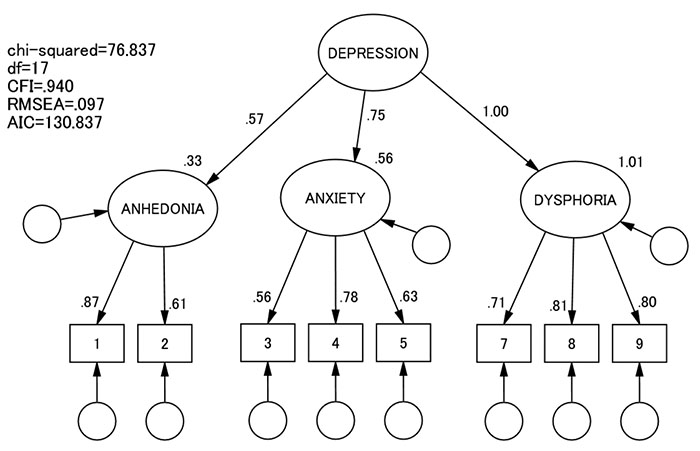
[http://dx.doi.org/10.1111/j.1467-6494.2011.00749.x] [PMID: 2209 1867] ]. In a higher-order factor model (also known as a second-order model or an indirect hierarchical model), as in the single- or first-order factor models, each indicator is influenced by one of the first-order factors. In addition, each first-order factor is influenced by the general factor (Fig. 4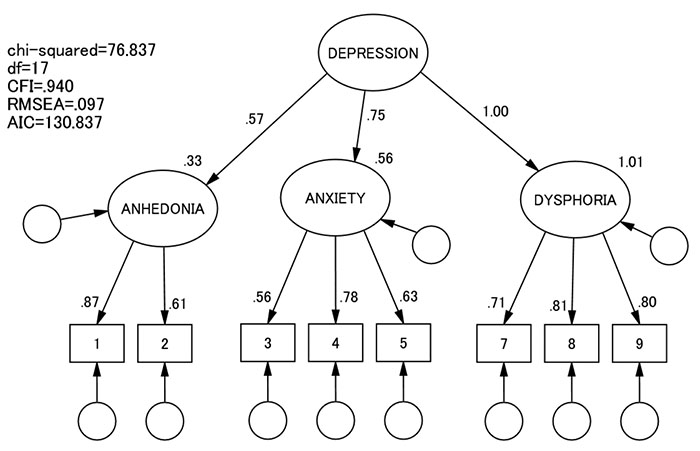 ). The shared variance of the higher-order factors is accounted for by the second-order general factor, which is unlikely with the first-order factor models. In other words, the first-order factor model assumes that factors are correlated and that the construct (e.g., postnatal depression) is multidimensional and explained by obliquely related dimensions. In contrast, the second-order model assumes that the factors are uncorrelated and represented by a general depression construct. Therefore, the general factor influences each indicator indirectly via first-order factors.
). The shared variance of the higher-order factors is accounted for by the second-order general factor, which is unlikely with the first-order factor models. In other words, the first-order factor model assumes that factors are correlated and that the construct (e.g., postnatal depression) is multidimensional and explained by obliquely related dimensions. In contrast, the second-order model assumes that the factors are uncorrelated and represented by a general depression construct. Therefore, the general factor influences each indicator indirectly via first-order factors.
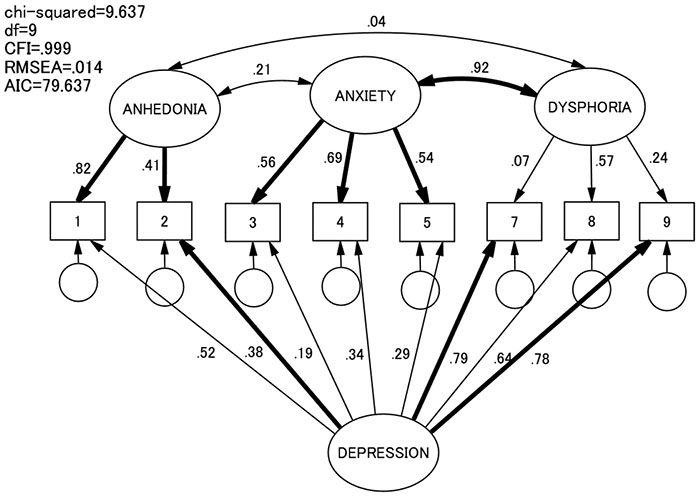
In the bifactor model (also known as a hierarchical factor model or an indirect hierarchical factor model), the general factor influences all the indicators directly but not via the first-order factors (Fig. 5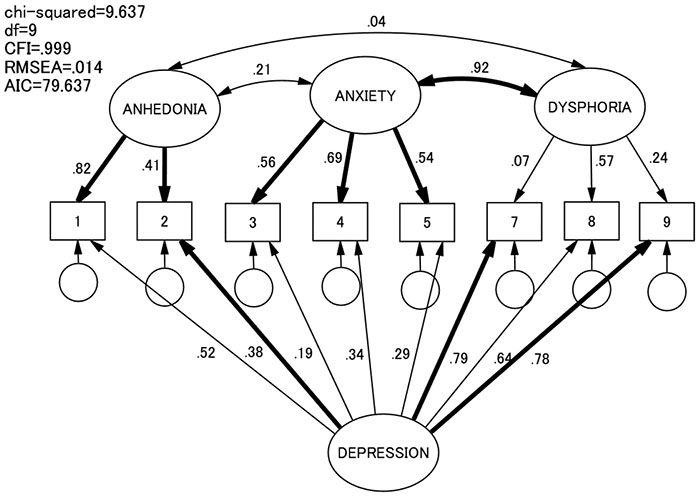 ). The idea is that all the indicators differ according to the general factor, whereas groups of indicators are dependent on each first-factor they belong to independently from the influence of the general factor. Here, the general factor and the first-order factors are independent of each other. For example, an indicator (e.g., “cannot see the funny side of things” is a reflection of a specific aspect (e.g., anhedonia) as well as the general severity (of depression). In our study, we compared different models of EPDS factor structures. We also compared our models with that proposed by Kubota et al. [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
). The idea is that all the indicators differ according to the general factor, whereas groups of indicators are dependent on each first-factor they belong to independently from the influence of the general factor. Here, the general factor and the first-order factors are independent of each other. For example, an indicator (e.g., “cannot see the funny side of things” is a reflection of a specific aspect (e.g., anhedonia) as well as the general severity (of depression). In our study, we compared different models of EPDS factor structures. We also compared our models with that proposed by Kubota et al. [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ].
The above argument implies not only statistical precision but also causal as well as consequential issues. For example, even though scores of a subscale were correlated with a possible predictor, it may be a spurious product confounded by the general factor. Such a hypothesis can be examined by Structural Equation Modelling (SEM) where the external variable (a predictor) sends paths to the subscale factors and the general factor (Fig. 6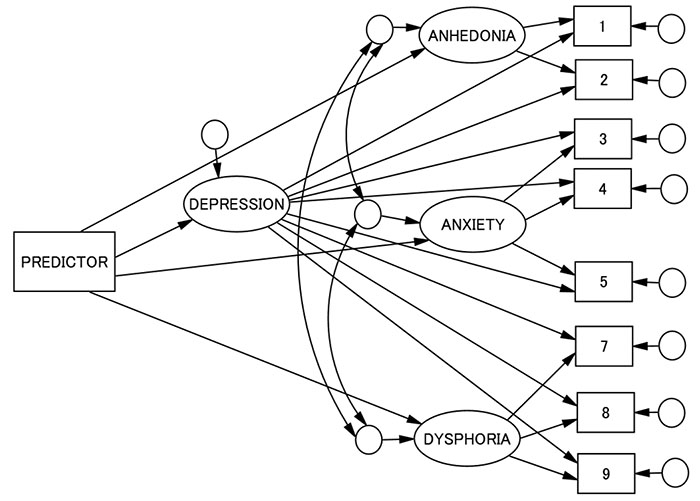 ). Also, the case is the influence of specific and general factors on outcome variables (e.g., parenting difficulties in the case of PND). Our study tries to explore different associations of the factor structure we identify as the best fit with the data with demographic, obstetric, and psychosocial variables. We consider that such results may contribute to the construct validity of the model statistically identified [29Messick S. Validity of psychological assessment: Validation of inferences from persons’ responses and performances as scientific inquiry into score meaning. Am Psychol 1995; 50(9): 741-9.
). Also, the case is the influence of specific and general factors on outcome variables (e.g., parenting difficulties in the case of PND). Our study tries to explore different associations of the factor structure we identify as the best fit with the data with demographic, obstetric, and psychosocial variables. We consider that such results may contribute to the construct validity of the model statistically identified [29Messick S. Validity of psychological assessment: Validation of inferences from persons’ responses and performances as scientific inquiry into score meaning. Am Psychol 1995; 50(9): 741-9.
[http://dx.doi.org/10.1037/0003-066X.50.9.741] ].
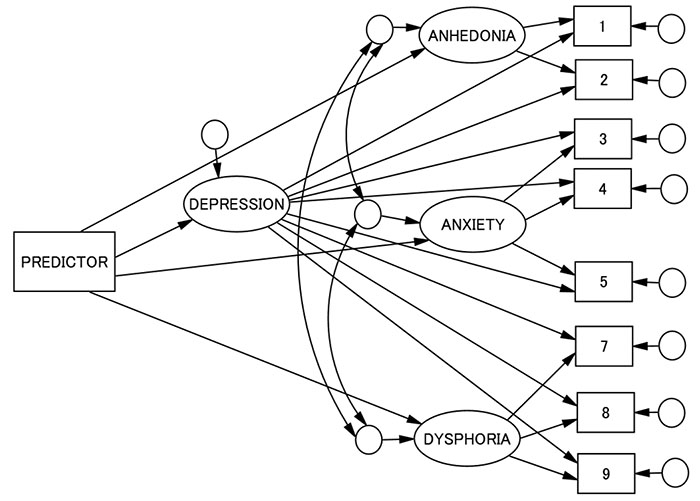 |
Fig. (6) Predictors and the EPDS general and subscale scores. The names of error variables are deleted. |
In this study, we selected variables related to Negative Life Events (NLEs) occurring after childbirth and coping styles and behaviours as external indicators. The postnatal period may be characterised as a life stage with many stressors. This period sees a dynamic role transition related to the parental role, adaptation to physical changes, and altered relationships with the spouse, other children, co-workers, or significant others [30Condon JT, Boyce P, Corkindale CJ. The First-Time Fathers Study: A prospective study of the mental health and wellbeing of men during the transition to parenthood. Aust N Z J Psychiatry 2004; 38(1-2): 56-64.
[http://dx.doi.org/10.1177/000486740403800102] [PMID: 14731195] -38Simpson JA, Rholes WS, Campbell L, Tran S, Wilson CL. Adult attachment, the transition to parenthood, and depressive symptoms. J Pers Soc Psychol 2003; 84(6): 1172-87.]. Mothers of infants must adapt to the physical and social changes brought about by pregnancy, adopt their new role as a mother, and build new relationships. Hence, they are likely to experience emotional conflicts in themselves and social problems with others. Maternal identity should be established and mothers must learn new social skills to cooperate with others as well as to build a new family. Interpersonal conflict may manifest after childbirth. This may be related to childcare responsibilities and managing the newborn. This, coupled with a poor marital relationship, may lead to psychological maladjustment. Mothers may also have feelings of isolation because they have less time to communicate with other adults compared during non-childbearing periods. Thus, the postpartum period is stressful for women because of the increased incidence of these NLEs. This study explores specific associations that different aspects of PND symptomatology have with different types of NLEs.
Coping is the perception or behaviours people have or take when expecting or facing NLEs [39Lazarus RS, Folkman S. Stress, appraisal, and coping 1984., 40Snyder CR, Ford CE, Eds. Coping with negative life events: Clinical and social psychological perspectives 1987.
[http://dx.doi.org/10.1007/978-1-4757-9865-4] ]. The concept of coping has two components [41Beutler LE, Moos RH, Lane G. Coping, treatment planning, and treatment outcome: discussion. J Clin Psychol 2003; 59(10): 1151-67.
[http://dx.doi.org/10.1002/jclp.10216] [PMID: 12968279] , 42Moos RH, Holahan CJ. Dispositional and contextual perspectives on coping: toward an integrative framework. J Clin Psychol 2003; 59(12): 1387-403.
[http://dx.doi.org/10.1002/jclp.10229] [PMID: 14618606] ]. One is a stable coping style or styles that characterise an individual’s reactions to stressful situations. Another is a set of skills or techniques (coping behaviours) that people use to manage specific stressful situations. The former is dispositional and is part of ones personality [43O'Brien TB, DeLongis A. The interactional context of problem-, emotion-, and relationship-focused coping: The role of the big five personality factors. J Pers 1996; 64(4): 775-813., 44Vollrath M, Torgersen S, Alnæs R. Personality as long-term predictor of coping. Pers Individ Dif 1995; 18(1): 117-25.
[http://dx.doi.org/10.1016/0191-8869(94)00110-E] ]. In contrast, the coping behaviours may be determined more by one’s current situation [45McCrae RR. Situational determinants of coping responses: Loss, threat, and challenge. J Pers Soc Psychol 1984; 46(4): 919-28.
[http://dx.doi.org/10.1037/0022-3514.46.4.919] [PMID: 6737200] ]. The choice of coping behaviours is determined by the specificity of a situation. The coping styles and coping behaviours are moderately correlated [46Shikai N, Nagata T, Kitamura T. Do people cope with situations as they say? Relationship between perceived coping style and actual coping response. Psychiatry Clin Neurosci 2014; 68(2): 154-9.
[http://dx.doi.org/10.1111/pcn.12094] [PMID: 24118236] ]. This study explores specific associations that different aspects of PND symptomatology have with different aspects of coping characteristics.
These methodological considerations based on the recent development of statistics related to factor structure prompted us to reanalyse the data we collected in the previous studies conducted several years ago.
2. METHODS
2.1. Study Procedures and Participants
Data came from a two-wave follow-up study on PND among women who gave birth at five antenatal clinics in Okayama City, Japan, between August 2000 and March 2001. One of the clinics was a university hospital, whereas the other four were private clinics. One thousand five hundred and thirty women were eligible for this study. Among them, 1,200 (78%) women received the questionnaires, and 758 (63%) returned the questionnaires at both waves. Our analyses were based on these 758 women’s reports. The mean (SD) age of the participants was 28.7 (4.1) years and the mean age (SD) of their partners was 30.7 (5.2) years.Among them, 47%of the infants were boys. The mean body weight (SD) of the infants was 3,050 (347) g. Approximately 85% of the women gave birth vaginally, while the others required delivery by vacuum extraction (7%) and caesarean section (7%), respectively. Of these women, 234 (31%) had already boys and 210 (28%) had already had girls. The mean (SD) age was 3.5 (2.6) for the oldest boy child and 3.7 (2.5) for the oldest girl child. About 80% of the boys the women had already had were aged less than 5 and 76% of the girls the women had already had were aged less than 5. We were unable to obtain demographic data such as the age and parity of mothers who refrained from the study for ethical reasons.
2.2. Measurements
Postnatal depression: We used the EPDS (Cox et al., 1987) [13Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987; 150(6): 782-6.
[http://dx.doi.org/10.1192/bjp.150.6.782] [PMID: 3651732] ], which consists of 10itemswith a four-point scale(0 to 3). The original English version of the EPDS had good internal consistency (Cronbach’s alpha = 0.87) and reliability (split-half reliability = 0.88). The EPDS was introduced to Japan by Okano et al. [14Okano T, Murata M, Masuji F, et al. Validation and reliability of Japanese version of the EPDS. Arch Psychiatr Diagn Clin Evaluation 1996; 74: 525-33. [in Japanese].] through the forward-backwards translation procedure. The Japanese version of the EPDS has good internal consistency (Cronbach’s alpha = 0.78) and test-retest reliability (Spearman correlation = 0.92 [14Okano T, Murata M, Masuji F, et al. Validation and reliability of Japanese version of the EPDS. Arch Psychiatr Diagn Clin Evaluation 1996; 74: 525-33. [in Japanese].].
Negative life events: We selected 41events that may appear after childbirth based on a report by [47Arizmendi TG, Affonso DD. Stressful events related to pregnancy and postpartum. J Psychosom Res 1987; 31(6): 743-56.
[http://dx.doi.org/10.1016/0022-3999(87)90023-7] [PMID: 3430433] ]. We added a few items suitable for Japanese culture. These Negative Life Events (NLEs) were categorized into four life domains:(a) Physical Symptoms and Body Image (13 items); (b) Lifestyle Changes and Financial Problems (10 items); (c) Interpersonal Relationships and Out-of-Home Activities (10 items);and (d) Parenting and Newborn Behaviours (eight items) [48Ohashi Y, Takegata M, Haruna M, Kitamura T, Takauma F, Tada K. Association of specific negative life events with depression severity one month after childbirth in community-dwelling mothers. Int J Nurs Health Sci 2015; 2(2): 13-20.]. The participants were asked whether they had experienced any of these events since childbirth, and if so, to measure their desirable or undesirable impact using a 100-point scale. If the event was desirable, it was rated using a positive value (e.g., +78), whereas if undesirable, the event was rated using a negative value (e.g., – 46). If the event did not occur after childbirth, or if it did occur but caused neither a negative nor a positive impact, it was rated as zero (0).
Coping styles and behaviours: Kendler et al. [49Kendler KS, Kessler RC, Heath AC, Neale MC, Eaves LJ. Coping: A genetic epidemiological investigation. Psychol Med 1991; 21(2): 337-46.
[http://dx.doi.org/10.1017/S0033291700020444] [PMID: 1876639] ] selected 14 items from the Ways of Coping Checklist (WCCL;Folkman & Lazarus, 1985 [50Folkman S, Lazarus RS. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. J Pers Soc Psychol 1985; 48(1): 150-70.
[http://dx.doi.org/10.1037/0022-3514.48.1.150] [PMID: 2980281] ]) based on the highest-loading items from each of the seven subscales. Following the factor loadings of these WCCL items, Kendler et al. [49Kendler KS, Kessler RC, Heath AC, Neale MC, Eaves LJ. Coping: A genetic epidemiological investigation. Psychol Med 1991; 21(2): 337-46.
[http://dx.doi.org/10.1017/S0033291700020444] [PMID: 1876639] ] grouped them into three categories. They included Turning to Others (four items, e.g., ‘turn to friends or relatives for advice or assistance’), Problem Solving (six items, e.g., ‘confront the person who caused the problem’), and Denial (three items, e.g., ‘try not to think about it so much’). We followed this procedure to measure both perceived coping styles and enacted coping behaviours. At fivedays after childbirth, we asked the participant how ‘she usually copes with a difficult situation’ using a five-point scale from ‘never’ (1) to ‘very often’ (5) (perceived coping styles). At one month after childbirth, we asked the participant how she coped with the event she rated as being the most stressful during the time since childbirth using a five-point scale (enacted coping behaviours).
Demographic and obstetric variables: We asked the participant’s age and parity. We also enquired about the neonate’s body weight and gender (boy – 1; girl – 2) and perceived difficulty of the current labour using a three-point scale, from ‘less than expected’ (1) to ‘more than expected’ (3).
2.3. Data Analysis
The whole sample (N = 758) was divided randomly into two parts: one (n = 380) for EFAs and another (n = 378) for CFAs. This procedure was conducted via SPSS ‘case selection’. For the first group, we first examined the Kaiser-Meyer-Olkin (KMO) index and Bartlett’s sphericity test to perform a factorability check [51Burton LJ, Mazerolle SM. Survey instrument validity Part I: Principles of survey instrument development and validity in athletic training education research. Athletic Training Education J 2011; 6(1): 27-35.] The communality and skewness of all the EPDS items were also examined. We next performed a series of EFAs by the maximum-likelihood method with PROMAX rotation from a single-factor structure and, subsequently, models with an increasingly greater number of factors (i.e., two-, three-factor structures, and so on).
Next, we compared the goodness-of-fit of these models in a series of CFAs using the second halved sample. This was the cross-validation of the models derived from EFAs. Here, we also added the three-factor model proposed by Kubota et al. [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ].The fit of models with the data was examined in terms of chi-squared (χ2), the Comparative Fit Index (CFI), and the Root Mean Square Error of Approximation (RMSEA). Starting from the single-factor model, the subsequent model was judged better if its χ2 value was significantly lower than that for the former model. According to conventional criteria, a good fit would be indicated by χ2/df < 2, CFI > 0.97, and RMSEA < 0.05, and an acceptable fit by χ2/df< 3, CFI >0.95, and RMSEA < 0.08 [52Bentler PM. Comparative fit indexes in structural models. Psychol Bull 1990; 107(2): 238-46.
[http://dx.doi.org/10.1037/0033-2909.107.2.238] [PMID: 2320703] , 53Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online 2003; 8(2): 23-74.] We also used the Akaike information criterion (AIC;Akaike, 1987 [54Akaike H. Factor analysis and AIC. Psychometrika 1987; 52(3): 317-32.
[http://dx.doi.org/10.1007/BF02294359] ]), where a lower AIC was judged as being better.
Having selected the best-fit model, the second-order and bifactor models were examined. These models were reconciliation of the unidimensional and multidimensional models [28Brunner M, Nagy G, Wilhelm O. A tutorial on hierarchically structured constructs. J Pers 2012; 80(4): 796-846.
[http://dx.doi.org/10.1111/j.1467-6494.2011.00749.x] [PMID: 2209 1867] , 55Chen FF, Hayes A, Carver CS, Laurenceau JP, Zhang Z. Modeling general and specific variance in multifaceted constructs: A comparison of the bifactor model to other approaches. J Pers 2012; 80(1): 219-51.
[http://dx.doi.org/10.1111/j.1467-6494.2011.00739.x] [PMID: 2209 2195] -58Reise SP, Morizot J, Hays RD. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Qual Life Res 2007; 16(Suppl. 1): 19-31.
[http://dx.doi.org/10.1007/s11136-007-9183-7] [PMID: 17479357] ]. Again, we selected the model that showed a significant decrease in χ2 value compared with the other models.
After identifying the model that had the best fit with the data, we calculated subscale scores using this factor structure selected as the best one. The new subscales derived from such procedures were correlated with the other variables including demographic and obstetric variables, NLEs that occurred after childbirth, and coping styles and behaviours. Identifying those variables with significant correlations (p < .001 because of multiple comparisons) with the EPDS subscale scores, we examined the impacts of these variables in a structural regression model using a structural equation model (SEM) (Fig. 6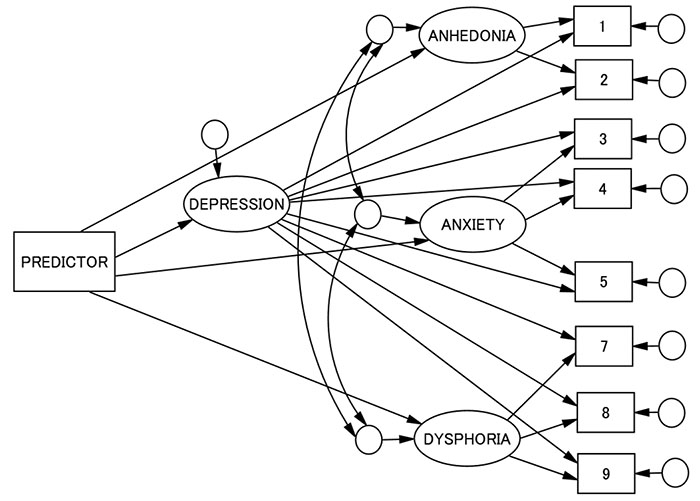 ).
).
Hence, our research questions were two-fold: (1) what would be the best factor structure of the EPDS in a Japanese population, and (2) how was the construct validity of such factor structure.
2.4. Ethical Consideration
All participants asked to participate in this study were provided with a document that explained the aim and procedure of this study and the confidentiality of personal information. Participants were regarded as agreeing to participate by returning the questionnaire to the responsible researcher (T.K.) via postal service. This study was conducted under the approval of the Ethical Committee of the National Institute of Mental Health, Konodai Campus, where the responsible researcher (T.K.) was working while the study was conducted.
3. RESULTS
3.1. EFA
The KMO index was 0.828 and Bartlett’s sphericity test showed a significant result (p < .001) in the first halved sample. Communalities of the EPDS items were generally good except for item 6 (Table 2). All the EPDS items were not extremely skewed except for item 10 (suicidal idea) (Table 2). Thus, the data were considered adequate to proceed to EFAs. A scree plot indicated a possible three-factor structure (Fig. 7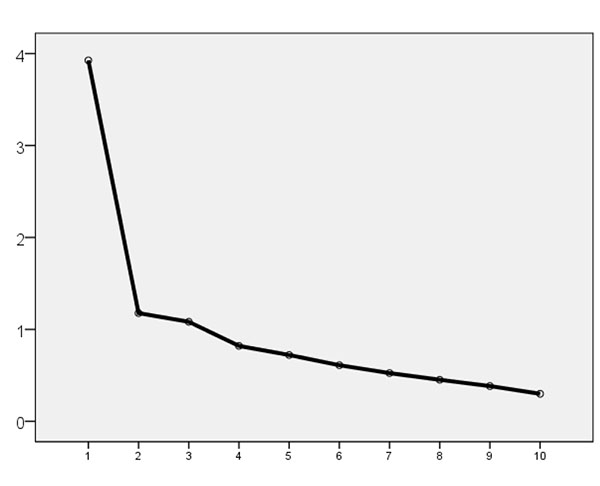 ). Nevertheless, because of the idiosyncrasy of the number of the factors in EFAs, we calculated factor loadings of EPDS items in single-, two-, and three-factor structures (Table 3).
). Nevertheless, because of the idiosyncrasy of the number of the factors in EFAs, we calculated factor loadings of EPDS items in single-, two-, and three-factor structures (Table 3).
In the single-factor structure, all the items showed factor loading > 0.3 [26Costello AB, Osborne JW. Best practices in explanatory factor analysis: Four recommendations for getting the most from your analysis. Pract Assess, Res Eval 2005; 10(7): 1-9.]. In the two-factor model, two items of loss of interest (items 1 and 2) were loaded on the second factor, while the first factor was loaded on all the remaining items. Here, item 6 showed a slightly low factor loading (0.26). In the three-factor structure model, the first factor of the two-factor model was divided into two. In the three-factor model, items 5, 7, 9, and 10, reflecting unhappiness and suicidal thoughts,were loaded on the first factor. Items 1 and 2, reflecting the loss of interest, were loaded on the second factor. The last factor was loaded on items 3, 4, 6, and 8, reflecting anxiety and self-blame (Table 3).
3.2. CFA
Having obtained single-, two-, and three-factor models derived from EFAs, we used the second halved sample to determine the goodness-of-fit for all three models. This was a cross-validation of the EFA-derived factor structure in order to identify the extent to which the scale’s factor structure was stable. The decrease of χ2 was significant from the single- to two-factor models (Table 4) as well as from the two- to three-factor models. Furthermore, we calculated the fit indices of the three-factor model proposed by Kubota et al. (2014) [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ]. This showed a significant decrease in χ2 value from our three-factor model. The AIC of the three-factor model of Kubota et al. (2014) [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
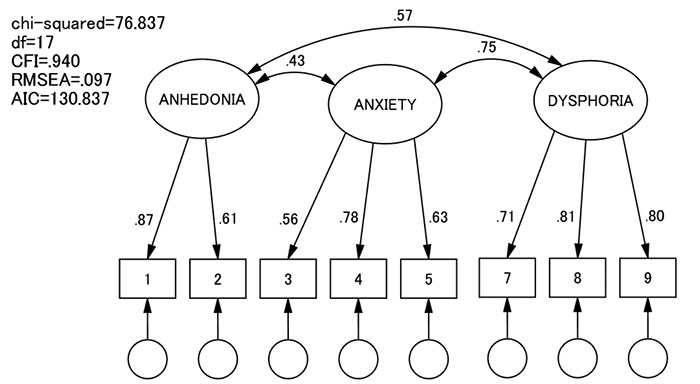
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ] was the lowest (best) among all the models. Hence, we adopted this model. In this model, items 1 and 2 reflected loss of interest; items 3, 4, and 5 reflected the anxious mood, panic, and self-blame; and items 7, 8, and 9 reflected unhappy mood and sadness (Fig. 8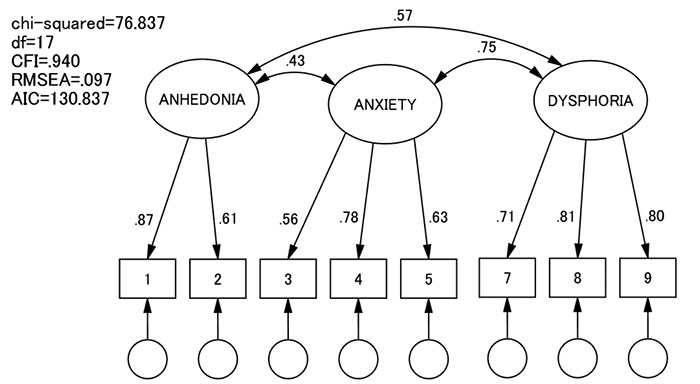 ). We named these three factors anhedonia, anxiety, and dysphoria. The last factor was named depression by Kubota et al. (2014) [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
). We named these three factors anhedonia, anxiety, and dysphoria. The last factor was named depression by Kubota et al. (2014) [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ], but we renamed it to dysphoria because we reserved ‘depression’ as an indication of the severity of PND reflected by the total EPDS scores (see below). This model was, though the best among the first-order factor structure models, still not very good in its fit with the data: χ2/df = 4.52, CFI = 0.940, and RMSEA = 0.097.
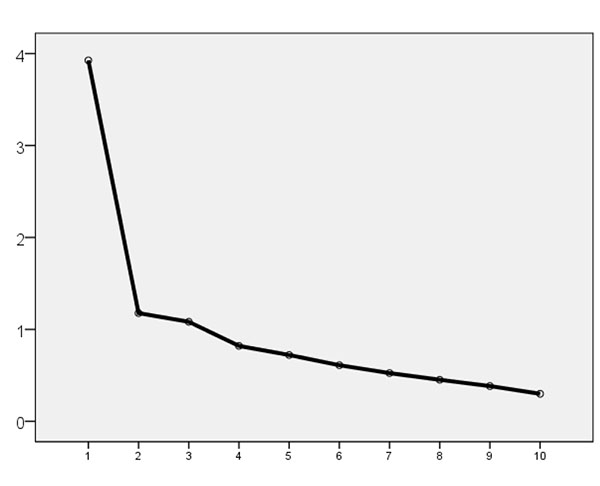 |
Fig. (7) Scree plot of the EFA of the EPDS items. |
Next, we examined second-order (hierarchical) and bifactor models that were adapted in the three-factor model of Kubota et al. (2014) [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ] (Table 4). The second-order (hierarchical) model was an inappropriate solution (Fig. 4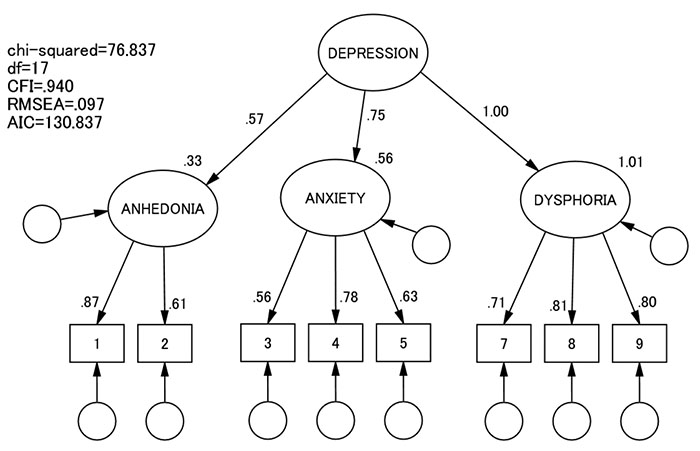 ). We found that the bifactor model showed a much better fit with data than the first-order three-factor model: χ2/df = 1.07, CFI = 0.999, RMSEA = 0.14, and AIC = 79.637 (Fig. 5
). We found that the bifactor model showed a much better fit with data than the first-order three-factor model: χ2/df = 1.07, CFI = 0.999, RMSEA = 0.14, and AIC = 79.637 (Fig. 5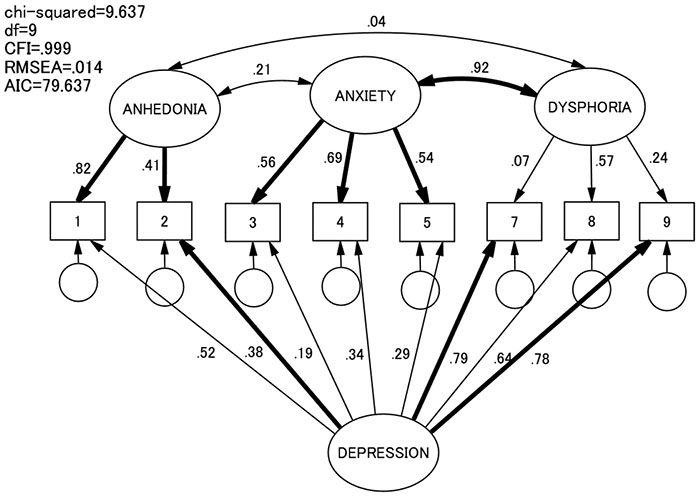 ).Therefore, we adopted the bifactor Kubota model as our final model.
).Therefore, we adopted the bifactor Kubota model as our final model.
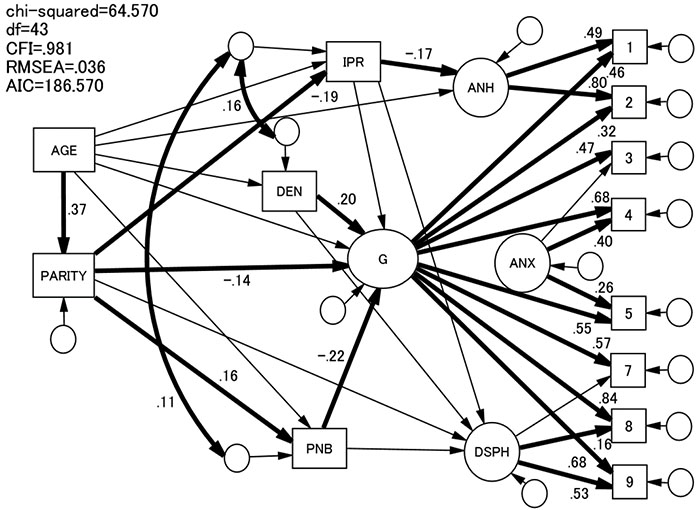
3.3. Predictors of the EPDS Factors
We calculated three subscale scores-anhedonia, anxiety, and dysphoria-derived from the final bifactorial model as well as the total scores of the eight EPDS items (general depression). These subscale and general scores were correlated with the other variables (Table 5). General depression was significantly predicted by Parenting and Newborn Behaviours, Enacted Problem Solving and Enacted Turning to Others. Anhedonia was significantly predicted by Interpersonal Relationships and Out-of-Home Activities, as well as Parenting and Newborn Behaviours. Anxiety was predicted by younger age, parity (nulliparousness), Parenting and Newborn Behaviours, enacting Problem Solving, and Turning to Others. Dysphoria was predicted by Interpersonal Relationships and Out-of-Home Activities, Parenting and Newborn Behaviours, Enacting Denial, and Enacting Problem Solving.
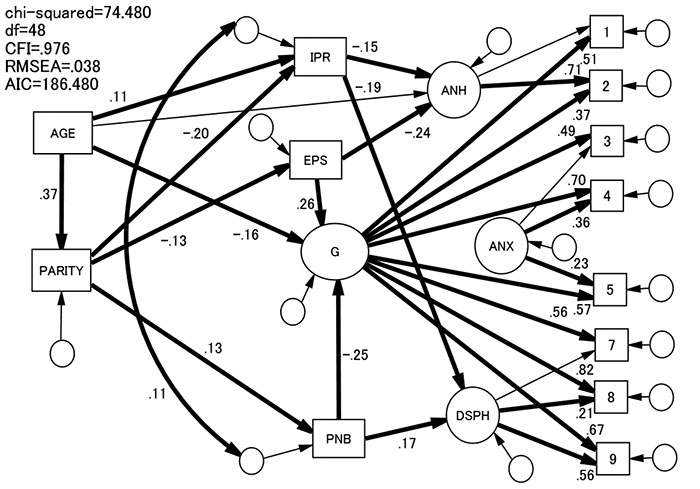
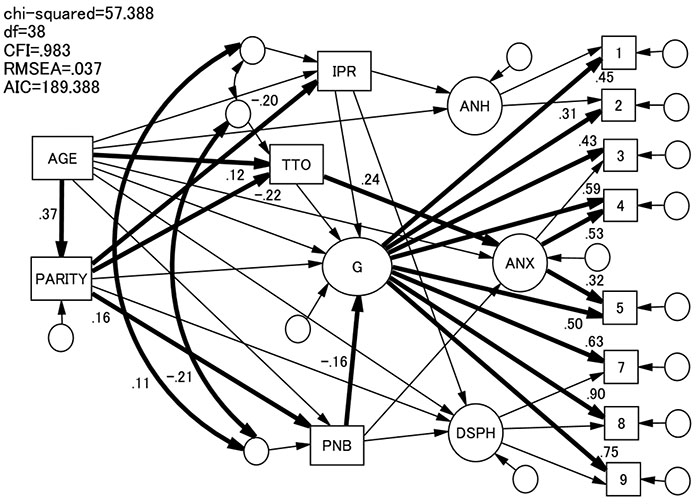
We selected the variables that were significantly correlated with the EPDS subscale and general scores (p < .001) to build an SEM model (Figs. 9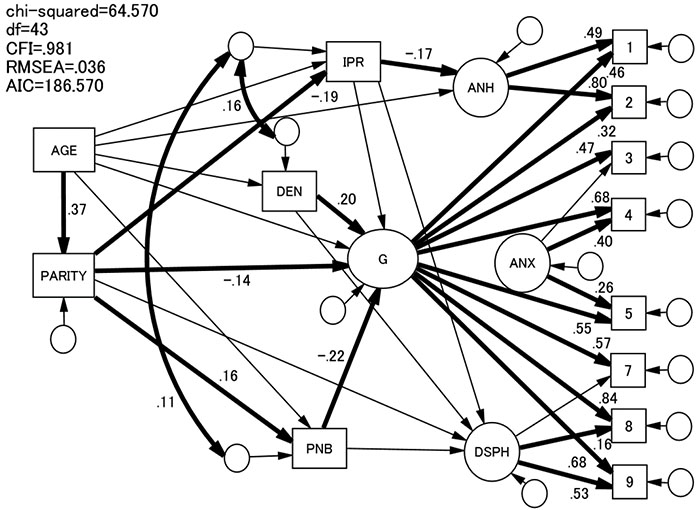 , 10
, 10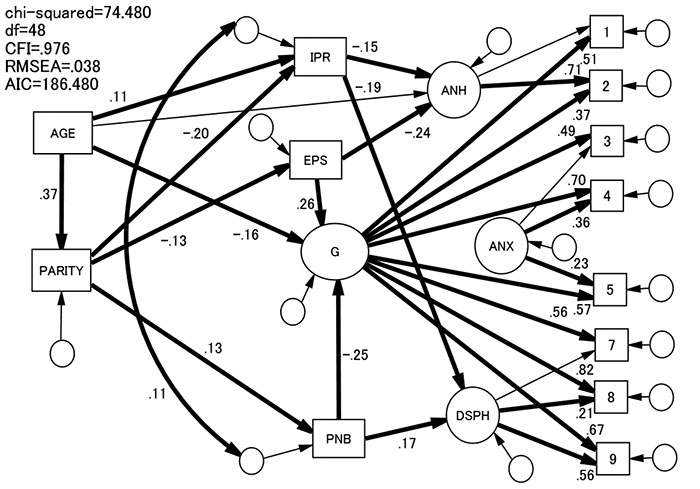 , and 11
, and 11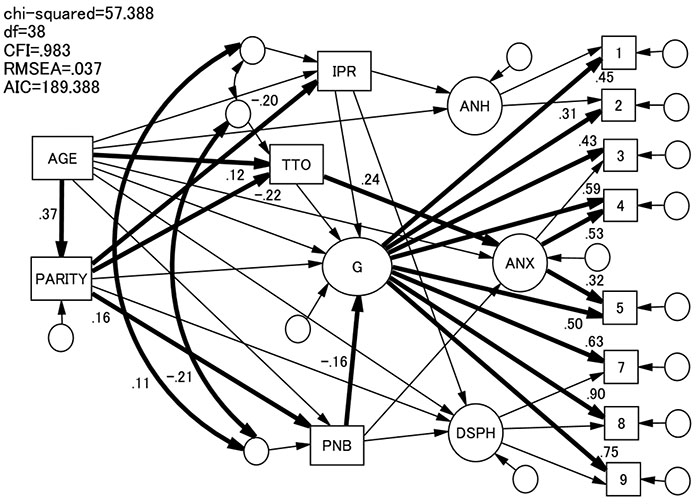 ). Here, we examined the effects of three types of enacted coping behaviours (Enacted Denial, Enacted Problem Solving, and Enacted Turning to Others) separately.
). Here, we examined the effects of three types of enacted coping behaviours (Enacted Denial, Enacted Problem Solving, and Enacted Turning to Others) separately.
In SEMs, we posited that (1) age would predict parity, NLEs (i.e., Interpersonal Relationships and Out-of-Home Activities, and Parenting and Newborn Behaviours), each of the enacted coping behaviours (i.e., Enacted Problem Solving, Enacted Denial, Enacted Turn to Others), and the subscale and general scores of the EPDS; (2) parity would predict NLEs, coping behaviours, and the subscale and general scores of the EPDS; (3) NLEs would predict the subscale and general scores of the EPDS; (4) each coping behaviour would predict the subscale and general scores of the EPDS; (5) NLEs were correlated with each other; and (6) the coping behaviour would be correlated with NLEs.
In each of the SEMs, we trimmed models by deleting the least significant path one by one until there were no non-significant paths or the model trimming produced a statistically significant (p < .05) χ2 increase or an inappropriate solution occurred [59Klein RB. Principles and practice of structural equation modelling 3rd ed. 2011.].
Our final models showed a good fit with the data: enacted denial model χ2/df = 1.502, CFI = 0.981, RMSEA = 0.036, AIC = 186.570 (before trimming:χ2/df = 1.823, CFI = 0.976, RMSEA = 0.047, AIC = 202.156) (Fig. 9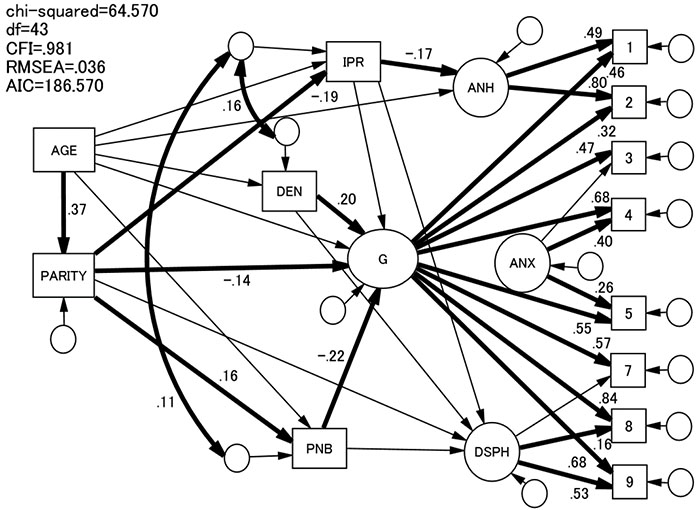 ); enacted problem solving model χ2/df = 1.552, CFI = 0.976, RMSEA = 0.038, AIC = 186.480 (before trimming: χ2/df = 1.799, CFI = 0.977, RMSEA = 0.046, AIC = 201.360) (Fig. 10
); enacted problem solving model χ2/df = 1.552, CFI = 0.976, RMSEA = 0.038, AIC = 186.480 (before trimming: χ2/df = 1.799, CFI = 0.977, RMSEA = 0.046, AIC = 201.360) (Fig. 10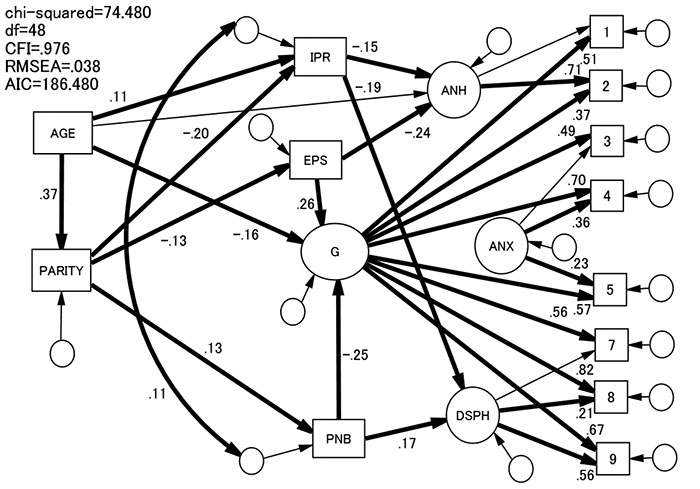 ); enacted turning to others model χ2/df = 1.510, CFI = 0.983, RMSEA = 0.037, AIC = 189.388 (before trimming: χ2/df = 1.729, CFI = 0.983, and RMSEA = 0.037, AIC = 189.388) (Fig. 11
); enacted turning to others model χ2/df = 1.510, CFI = 0.983, RMSEA = 0.037, AIC = 189.388 (before trimming: χ2/df = 1.729, CFI = 0.983, and RMSEA = 0.037, AIC = 189.388) (Fig. 11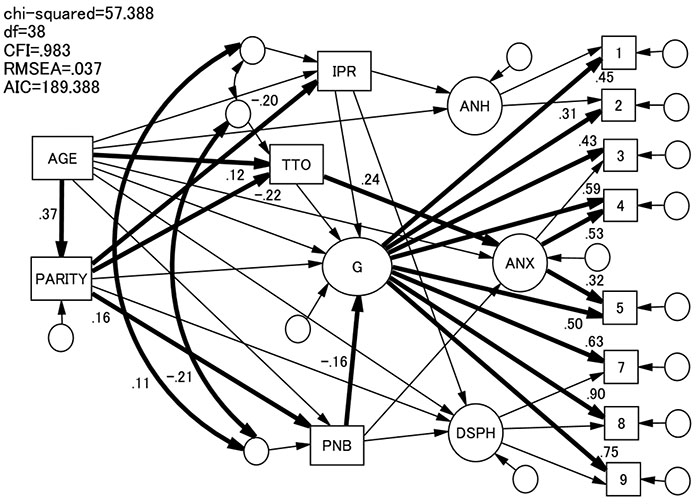 ). General depression was significantly predicted by Parenting and Newborn Behaviours in each case. It was also predicted positively by Enacted Problem Solving and Enacted Denial. Anhedonia was significantly predicted by Interpersonal Relationships and Out-of-Home Activities, and (lack of) Enacted Problem Solving. Anxiety was significantly positively predicted by Enacted Turning to Others. Dysphoria was significantly predicted by Interpersonal Relationships and Out-of-Home Activities, and positively predicted by Parenting and Newborn Behaviours.
). General depression was significantly predicted by Parenting and Newborn Behaviours in each case. It was also predicted positively by Enacted Problem Solving and Enacted Denial. Anhedonia was significantly predicted by Interpersonal Relationships and Out-of-Home Activities, and (lack of) Enacted Problem Solving. Anxiety was significantly positively predicted by Enacted Turning to Others. Dysphoria was significantly predicted by Interpersonal Relationships and Out-of-Home Activities, and positively predicted by Parenting and Newborn Behaviours.
Higher age predicted parity, Interpersonal Relationships and Out-of-Home Activities, and Turning to Others. Younger age also predicted greater PND severity. Nulliparity predicted Interpersonal Relationships and Out-of-Home Activities, whereas multiparity predicted Parenting and Newborn Behaviours. Nulliparous women were likely to use Enacted Problem Solving and Turning to Others. Nulliparousness also predicted severity of PND.
4. DISCUSSION
The present study showed that among the three-factor structure models of the full EPDS―the single-, two-, and three-factor models―the three-factor model showed the best fit with the model. However, the three-factor model of Kubota et al. (2014) [27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] ], which excluded items 6 ‘things have been getting on top of me’ and 10 ‘thought of harming myself’ fit better than ours. Item 6 showed a factor loading >0.3 in none of the three models in our study. This is in accordance with previous studies [22Tuohy A, McVey C. Subscales measuring symptoms of non-specific depression, anhedonia, and anxiety in the Edinburgh Postnatal Depression Scale. Br J Clin Psychol 2008; 47(Pt 2): 153-69.
[http://dx.doi.org/10.1111/j.2044-8260.2008.tb00463.x] [PMID: 177 61026] , 27Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941
[http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] , 60Cunningham NK, Brown PM, Page AC. Does the Edinburgh Postnatal Depression Scale measure the same constructs across time? Arch Women Ment Health 2015; 18(6): 793-804.
[http://dx.doi.org/10.1007/s00737-014-0485-9] [PMID: 25510935] ]. These results suggest that item 6 is unstable as an indicator of the EPDS. Item 10 showed a factor loading > 0.3, but it was skewed (> 3.0). Despite its clinical relevance (suicidality), its psychometric value may cast doubt on its use as a screening instrument or indicator of PND severity.
Another unique factor of our study is the application of the bifactor model. This resulted in an extremely better fit of the model with the data. Reichenheim et al. [61Reichenheim ME, Moraes CL, Oliveira AS, Lobato G. Revisiting the dimensional structure of the Edinburgh Postnatal Depression Scale (EPDS): Empirical evidence for a general factor. BMC Med Res Methodol 2011; 11: 93.
[http://dx.doi.org/10.1186/1471-2288-11-93] [PMID: 21689442] ] proposed bifactor modes of EPDS using 10 items and suggested that using all EPDS items is suited to clinical practices. However, our model, which consists of eight items, showed better fit indices than the three-factor model with all 10 items. A scale that consists of fewer items is usually more useful for clinicians. Therefore, we recommend using the eight-item version. This model comprised a single general dimension alongside three distinct subfactors (anhedonia, anxiety, and dysphoria). The structural conceptualisation of PND in terms of a bifactor model should help us understand the interplay between the general condition and dimensions of symptoms of PND.
Scrutiny of the factor loadings of this bifactor model indicates characteristics of PND symptomatology (Fig. 5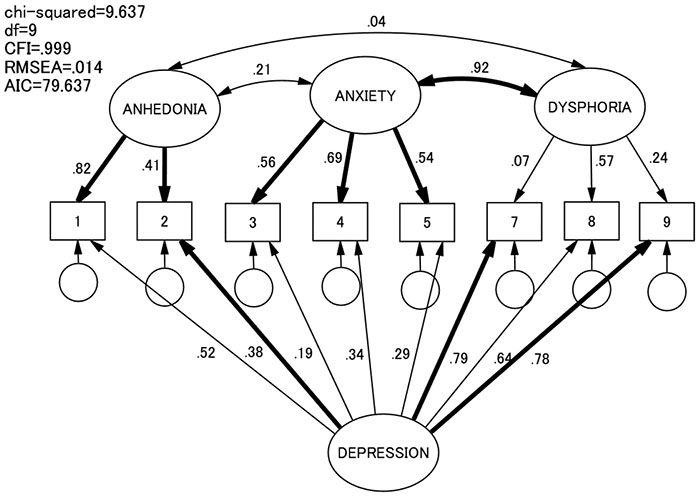 ). Although items 7, 8, and 9 were indicators of the dysphoria factor, their factor loadings were not significant. Items 7 and 9 were loaded on the general depression factor significantly. These findings may mean that these three items reflect the severity of PND, in general, more than the specific aspect of dysphoria. In contrast, items 3, 4, and 5 were loaded significantly on the anxiety factor but not significantly on the general depression factor. Hence, they may be more specific indicators, as are items 1 and 2, which were indicators of anhedonia. However, item 2 was significantly loaded on the general depression factor.
). Although items 7, 8, and 9 were indicators of the dysphoria factor, their factor loadings were not significant. Items 7 and 9 were loaded on the general depression factor significantly. These findings may mean that these three items reflect the severity of PND, in general, more than the specific aspect of dysphoria. In contrast, items 3, 4, and 5 were loaded significantly on the anxiety factor but not significantly on the general depression factor. Hence, they may be more specific indicators, as are items 1 and 2, which were indicators of anhedonia. However, item 2 was significantly loaded on the general depression factor.
As we expected, a single general dimension alongside three distinct subfactors (anhedonia, anxiety, and dysphoria) was predicted by different predictor variables. We identified five variables as predictors: Interpersonal Relationships and Out-of-Home Activities, Parenting and Newborn Behaviours, Enacted Problem Solving, Enacted Denial, and Enacted Turning to Others. As reported previously [48Ohashi Y, Takegata M, Haruna M, Kitamura T, Takauma F, Tada K. Association of specific negative life events with depression severity one month after childbirth in community-dwelling mothers. Int J Nurs Health Sci 2015; 2(2): 13-20.], among the four predictors related to NLEs, two were identified: (a) Interpersonal Relationships and Out-of-Home Activities;and (b) Parenting and Neonatal Behaviours. Two other NLEs-Physical Symptoms and Body Image, and Lifestyle Changes and Financial Problems-showed no association with the EPDS subscale and general scores. Therefore, PND symptomatology has a specificity of the life event type. Furthermore, the variable Interpersonal Relationships and Out-of-Home Activities was associated with anhedonia and dysphoria, whereas Parenting and Neonatal Behaviours was associated with the general severity of PND. The inverse relationship between Parenting and Neonatal Behaviours and dysphoria is difficult to interpret (Fig. 10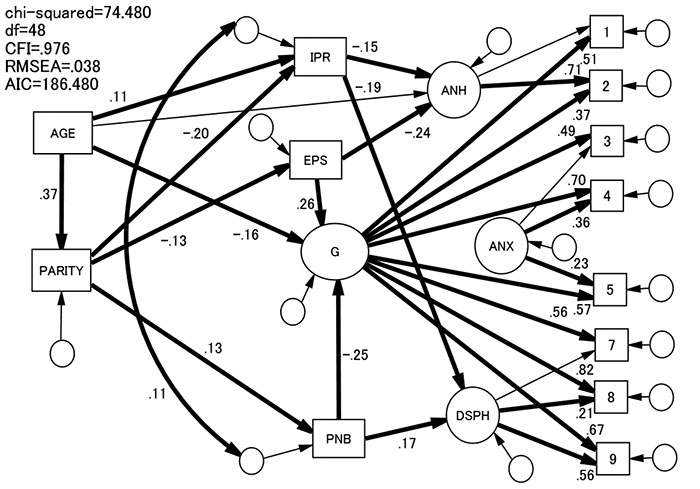 ). Excessive crying and feeding problems and infants’ sleeping problems were associated with mothers’ depression and anxiety [62Nolvi S, Karlsson L, Bridgett DJ, Pajulo M, Tolvanen M, Karlsson H. Maternal postnatal psychiatric symptoms and infant temperament affect early mother-infant bonding. Infant Behav Dev 2016; 43: 13-23.
). Excessive crying and feeding problems and infants’ sleeping problems were associated with mothers’ depression and anxiety [62Nolvi S, Karlsson L, Bridgett DJ, Pajulo M, Tolvanen M, Karlsson H. Maternal postnatal psychiatric symptoms and infant temperament affect early mother-infant bonding. Infant Behav Dev 2016; 43: 13-23.
[http://dx.doi.org/10.1016/j.infbeh.2016.03.003] [PMID: 27054496] -64Tikotzky L. Postpartum maternal sleep, maternal depressive symptoms and self-perceived mother-infant emotional relationship. Behav Sleep Med 2016; 14(1): 5-22.
[http://dx.doi.org/10.1080/15402002.2014.940111] [PMID: 25127316] ]. Our results suggest that such an association is through the increased PND severity rather than direct effects on the subscale dysphoria. It may be that difficulties associated with childrearing lead to more severe PND in general and when this is controlled, focusing on childcare may prevent women from paying attention to their own mood states [65Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. J Abnorm Psychol 2000; 109(3): 504-11.
[http://dx.doi.org/10.1037/0021-843X.109.3.504] [PMID: 11016119] -68Nolen-Hoeksema S, Parker LE, Larson J. Ruminative coping with depressed mood following loss. J Pers Soc Psychol 1994; 67(1): 92-104.
[http://dx.doi.org/10.1037/0022-3514.67.1.92] [PMID: 8046585] ].
The effects of age and parity on the EPDS subscale and general scores were mediated by these NLEs. First-time mothers were more likely to experience interpersonal problems, whereas mothers with more than one child were more likely to experience childrearing difficulties. The role transition from being a marital partner only to having a dual role as a wife and mother may be more stressful for first-time mothers, whereas rearing more than one baby simultaneously may be more stressful for mothers with multiple babies.
Enacted coping behaviours were differentially associated with the general and subscale scores of the EPDS. Thus, the general depression factor was more severe when the participants used denial and problem solving more frequently, whereas anhedonia was more severe when the participants used problem-solving less frequently. Anxiety was more severe when the participants used Turning to Others more frequently. The association between PND severity and denial as the coping behaviour may be due to the widely held notion that denial is a maladaptive coping strategy [69Terry DJ, Mayocchi L, Hynes GJ. Depressive symptomatology in new mothers: A stress and coping perspective. J Abnorm Psychol 1996; 105(2): 220-31.
[http://dx.doi.org/10.1037/0021-843X.105.2.220] [PMID: 8723003] ]. Of interest is the negative association between problem-solving and PND severity. This coping pattern is usually regarded as adaptive in many studies [50Folkman S, Lazarus RS. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. J Pers Soc Psychol 1985; 48(1): 150-70.
[http://dx.doi.org/10.1037/0022-3514.48.1.150] [PMID: 2980281] , 70Endler NS, Parker JD. Multidimensional assessment of coping: A critical evaluation. J Pers Soc Psychol 1990; 58(5): 844-54.
[http://dx.doi.org/10.1037/0022-3514.58.5.844] [PMID: 2348372] ]. People using problem-solving to cope in difficult situations carefully consider the causes of the difficulty and try to solve it by themselves. However, the NLEs experienced during the postnatal period are unique and often difficult to solve singlehandedly such as a baby’s cry in the night. In such a situation, the best coping strategy may be to ask for help from others. Thus, Turning to Others did not predict PND severity but, in our study, was associated with anxiety. Such behaviours may induce anxious moods, or, alternatively, anxious mothers may be likely to ask for help from others (e.g., their partner). Parity was also associated with coping behaviours. Thus, experienced mothers are likely to solve problems by themselves as well as ask for help from others.
We should discuss the clinical implications of our study. Our report suggests that parenting education and support in coping behaviours would be recommended as an intervention for PND. This is because of the severity of depression, in general, was significantly predicted by Parenting and Newborn Behaviours, Enacted Denial, and Enacted Problem Solving. Careful observation of a mother’s perceived difficulty with child care may encourage clinicians to provide child care assistance (e.g., support from family members and relatives, and NPOs such as Home Start). It has been reported that a doula’s emotional support enhances positive parenting and parent-child interactions [71Scott KD, Klaus PH, Klaus MH. The obstetrical and postpartum benefits of continuous support during childbirth. J Womens Health Gend Based Med 1999; 8(10): 1257-64.
[http://dx.doi.org/10.1089/jwh.1.1999.8.1257] [PMID: 10643833] , 72Thomas MP, Ammann G, Brazier E, Noyes P, Maybank A. Doula services within a healthy start program: Increasing access for an underserved population. Matern Child Health J 2017; 21(Suppl. 1): 59-64.
[http://dx.doi.org/10.1007/s10995-017-2402-0] [PMID: 29198051] ]. Continuous community-based support from the pregnancy to postnatal periods (e.g., home visiting) by doulas would be helpful. Neither denial nor problem solving should be recommended, but mothers should be advised to ask for support from others. Mothers may hesitate to ask for help from others. Nevertheless, excessive support seeking may be linked to anxiety. Anxious mothers who seek help from others excessively may be consulted in anxiety reduction. Difficulties with interpersonal relationships are another important clinical observation among first-time mothers in particular. Approaching these difficulties with interpersonal psychotherapy may be used as a means of intervention or prevention. Such ‘custom-made’ care and intervention may help mothers avoid PND.
Regarding the limitations of the present study, we should be cautious because this was based on only two observation points. Confounders of the results may be found in variables during the pregnancy period. Research should be extended to the whole perinatal period. NLEs after childbirth were rated by mothers themselves one month after birth simultaneously with the EPDS. The occurrence of NLEs may be a result of depression or anxiety [73Hammen C. Stress generation in depression: Reflections on origins, research, and future directions. J Clin Psychol 2006; 62(9): 1065-82.
[http://dx.doi.org/10.1002/jclp.20293] [PMID: 16810666] -75Wichers M, Maes HH, Jacobs N, Derom C, Thiery E, Kendler KS. Disentangling the causal inter-relationship between negative life events and depressive symptoms in women: A longitudinal twin study. Psychol Med 2012; 42(9): 1801-14.
[http://dx.doi.org/10.1017/S003329171100300X] [PMID: 22273464] ]. Mothers with anxiety or depression may perceive events as more stressful than other mothers. Neonatal behaviours should be rated independently by researchers, such as observation of a mother’s neonatal temperament. We were unable to make clinical diagnoses of mood and anxiety disorders. Detection of clinical cases may yield different findings. It was desirable to conduct a diagnostic interview with the mothers. Another point which needs further research is the scale’s cultural context. Obviously, we identified the factor structure of the EPDS only in Japanese culture (and language). We believe that the subscales we identified capture the different aspects of postnatal depression symptomatology. This should be compared with reports from the other cultures using different languages in the same framework of the factor structure.
CONCLUSION
Despite these drawbacks, our study expanded on a previous factor structural study of the EPDS and developed the multidimensional model. Also, this study explored different associations of the factor structure with psychological variables contributing to the construct validity of the model. The present results confirmed the presence of a general factor alongside anhedonia, anxiety, and dysphoria, presumably reflecting different aspects of the PND symptoms. Perinatal health care professionals should be encouraged to use the three subscales and the total EPDS score.
LIST OF ABBREVIATIONS
| PND | = Postnatal Depression |
| EPDS | = Edinburgh Postnatal Depression Scale |
| SEM | = Structural Equation Modelling |
| NLEs | = Negative Life Events |
| PCA | = Principal Component Analysis |
| RMSEA | = Root Mean Square Error of Approximation |
| CFI | = Comparative Fit Index |
| CFA | = Confirmatory Factor Analysis |
| AN | = Antenatal |
| SRMR | = Standardised Root Mean Square Residual |
| TLI | = Tucker-Lewis Index |
| AGFI | = Adjusted Goodness of Fit Index |
| df | = degrees of freedom |
| AIC | = Akaike Information Criteria |
| KMO | = Kaiser-Meyer-Olkin |
| DEN | = Enacted Denial |
| IPR | = Interpersonal Relationships |
| PNB | = Parenting and Newborn Behaviours |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The present study was approved by the Ethical Committee of Kumamoto University School of Medical Sciences References No. 458, where the last author (TK) conducted the present research.
HUMAN AND ANIMAL RIGHTS
No animals were used for studies that are the basis of this research.
CONSENT FOR PUBLICATION
All participants asked to participate in this study were provided with a document that explained the aim and procedure of this study and the confidentiality of personal information. Participants were regarded as agreeing to participate by returning the questionnaire to the responsible researcher.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We thank the following clinics for their cooperation: Okayama Central Hospital, Yamashita Clinic, Kohnan Ladies Clinic, Sunclinic, and Hashimoto Gynecologic and Obstetric Clinic.
REFERENCES
| [1] | American Psychiatric Association. Diagnostic and statistical manual of mental disorders 5th ed. 2013. |
| [2] | Beck CT. Predictors of postpartum depression: An update. Nurs Res 2001; 50(5): 275-85. [http://dx.doi.org/10.1097/00006199-200109000-00004] [PMID: 115 70712] |
| [3] | O’hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. Int Rev Psychiatry 1996; 8(1): 37-54. [http://dx.doi.org/10.3109/09540269609037816] |
| [4] | Kitamura T, Yoshida K, Okano T, et al. Multicentre prospective study of perinatal depression in Japan: Incidence and correlates of antenatal and postnatal depression. Arch Women Ment Health 2006; 9(3): 121-30. [http://dx.doi.org/10.1007/s00737-006-0122-3] [PMID: 16547826] |
| [5] | Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Women Ment Health 2005; 8(2): 77-87 . [http://dx.doi.org/10.1007/s00737-005-0080-1] |
| [6] | Moehler E, Brunner R, Wiebel A, Reck C, Resch F. Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother-child bonding. Arch Women Ment Health 2006; 9(5): 273-8. [http://dx.doi.org/10.1007/s00737-006-0149-5] [PMID: 16937313] |
| [7] | Wan MW, Green J. The impact of maternal psychopathology on child-mother attachment. Arch Women Ment Health 2009; 12(3): 123-34. [http://dx.doi.org/10.1007/s00737-009-0066-5] |
| [8] | Leiferman JA, Ollendick TH, Kunkel D, et al. Mothers' mental distress and parenting practices with infants and toddlers. Arch Women Ment Health 2005; 8(4): 243-47. |
| [9] | McLearn KT, Minkovitz CS, Strobino DM, Marks E, Hou W. Maternal depressive symptoms at 2 to 4 months post partum and early parenting practices. Arch Pediatr Adolesc Med 2006; 160(3): 279-84. [http://dx.doi.org/10.1001/archpedi.160.3.279] [PMID: 16520447] |
| [10] | Paulson JF, Dauber S, Leiferman JA. Individual and combined effects of postpartum depression in mothers and fathers on parenting behavior. Pediatrics 2006; 118(2): 659-68. [http://dx.doi.org/10.1542/peds.2005-2948] [PMID: 16882821] |
| [11] | Boyd RC, Le HN, Somberg R. Review of screening instruments for postpartum depression. Arch Women Ment Health 2005; 8(3): 141-53. [http://dx.doi.org/10.1007/s00737-005-0096-6] [PMID: 16133785] |
| [12] | Brodey BB, Goodman SH, Baldasaro RE, et al. Development of the Perinatal Depression Inventory (PDI)-14 using item response theory: a comparison of the BDI-II, EPDS, PDI, and PHQ-9. Arch Women Ment Health 2016; 19(2): 307-16. [http://dx.doi.org/10.1007/s00737-015-0553-9] [PMID: 26271280] |
| [13] | Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry 1987; 150(6): 782-6. [http://dx.doi.org/10.1192/bjp.150.6.782] [PMID: 3651732] |
| [14] | Okano T, Murata M, Masuji F, et al. Validation and reliability of Japanese version of the EPDS. Arch Psychiatr Diagn Clin Evaluation 1996; 74: 525-33. [in Japanese]. |
| [15] | Chen C, Gao J, Zhang J, Jia L, Yu T, Zheng Y. Serum leptin level measured 48 h after delivery is associated with development of postpartum depressive symptoms: A 3-month follow-up study. Arch Women Ment Health 2016; 19(6): 1001-8. [http://dx.doi.org/10.1007/s00737-016-0647-z] [PMID: 27295066] |
| [16] | Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ 2001; 323(7307): 257-60. [http://dx.doi.org/10.1136/bmj.323.7307.257] [PMID: 11485953] |
| [17] | Lupattelli A, Twigg MJ, Zagorodnikova K, et al. Self-reported perinatal depressive symptoms and postnatal symptom severity after treatment with antidepressants in pregnancy: A cross-sectional study across 12 European countries using the Edinburgh Postnatal Depression Scale. Clin Epidemiol 2018; 10: 655-69. [http://dx.doi.org/10.2147/CLEP.S156210] [PMID: 29922092] |
| [18] | Petrozzi A, Gagliardi L. Anxious and depressive components of Edinburgh Postnatal Depression Scale in maternal postpartum psychological problems. J Perinat Med 2013; 41(4): 343-8. [http://dx.doi.org/10.1515/jpm-2012-0258] [PMID: 23426862] |
| [19] | Takehara K, Tachibana Y, Yoshida K, Mori R, Kakee N, Kubo T. Prevalence trends of pre- and postnatal depression in Japanese women: A population-based longitudinal study. J Affect Disord 2018; 225: 389-94. [http://dx.doi.org/10.1016/j.jad.2017.08.008] [PMID: 28846961] |
| [20] | Berle JØ, Aarre TF, Mykletun A, Dahl AA, Holsten F. Screening for postnatal depression. Validation of the Norwegian version of the Edinburgh Postnatal Depression Scale, and assessment of risk factors for postnatal depression. J Affect Disord 2003; 76(1-3): 151-6. [http://dx.doi.org/10.1016/S0165-0327(02)00082-4] [PMID: 12943 945] |
| [21] | Guedeney N, Fermanian J. Validation study of the French version of the Edinburgh Postnatal Depression Scale (EPDS): New results about use and psychometric properties. Eur Psychiatry 1998; 13(2): 83-9. [http://dx.doi.org/10.1016/S0924-9338(98)80023-0] [PMID: 19698 604] |
| [22] | Tuohy A, McVey C. Subscales measuring symptoms of non-specific depression, anhedonia, and anxiety in the Edinburgh Postnatal Depression Scale. Br J Clin Psychol 2008; 47(Pt 2): 153-69. [http://dx.doi.org/10.1111/j.2044-8260.2008.tb00463.x] [PMID: 177 61026] |
| [23] | Small R, Lumley J, Yelland J, Brown S. The performance of the Edinburgh Postnatal Depression Scale in English speaking and non-English speaking populations in Australia. Soc Psychiatry Psychiatr Epidemiol 2007; 42(1): 70-8. [http://dx.doi.org/10.1007/s00127-006-0134-3] [PMID: 17102922] |
| [24] | Yong AG, Pearce S. A beginner’s guide to factor analysis: Focusing on exploratory factor analysis. Tutor Quant Methods Psychol 2013; 9(2): 79-94. [http://dx.doi.org/10.20982/tqmp.09.2.p079] |
| [25] | Ross LE, Gilbert Evans SE, Sellers EM, Romach MK. Measurement issues in postpartum depression part 1: Anxiety as a feature of postpartum depression. Arch Women Ment Health 2003; 6(1): 51-7. |
| [26] | Costello AB, Osborne JW. Best practices in explanatory factor analysis: Four recommendations for getting the most from your analysis. Pract Assess, Res Eval 2005; 10(7): 1-9. |
| [27] | Kubota C, Okada T, Aleksic B, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PLoS One 2014; 9(8)e103941 [http://dx.doi.org/10.1371/journal.pone.0103941] [PMID: 25089523] |
| [28] | Brunner M, Nagy G, Wilhelm O. A tutorial on hierarchically structured constructs. J Pers 2012; 80(4): 796-846. [http://dx.doi.org/10.1111/j.1467-6494.2011.00749.x] [PMID: 2209 1867] |
| [29] | Messick S. Validity of psychological assessment: Validation of inferences from persons’ responses and performances as scientific inquiry into score meaning. Am Psychol 1995; 50(9): 741-9. [http://dx.doi.org/10.1037/0003-066X.50.9.741] |
| [30] | Condon JT, Boyce P, Corkindale CJ. The First-Time Fathers Study: A prospective study of the mental health and wellbeing of men during the transition to parenthood. Aust N Z J Psychiatry 2004; 38(1-2): 56-64. [http://dx.doi.org/10.1177/000486740403800102] [PMID: 14731195] |
| [31] | Feeney J, Alexander R, Noller P, Hohaus L. Attachment insecurity, depression, and the transition to parenthood. Pers Relatsh 2003; 10(4): 475-93. [http://dx.doi.org/10.1046/j.1475-6811.2003.00061.x] |
| [32] | Levy-Shiff R. Individual and contextual correlates of marital change across the transition to parenthood. Dev Psychol 1994; 30(4): 591-601. [http://dx.doi.org/10.1037/0012-1649.30.4.591] |
| [33] | Lewis SNC, Cooper CL. The transition to parenthood in dual-earner couples. Psychol Med 1988; 18(2): 477-86. [http://dx.doi.org/10.1017/S0033291700008011] [PMID: 3399594] |
| [34] | Mercer RT, Nichols eg, Doyle GC. Transitions over the life cycle: A comparison of mothers and nonmothers. Nurs Res 1988; 37(3): 144-51. [http://dx.doi.org/10.1097/00006199-198805000-00004] [PMID: 336 8355] |
| [35] | Rholes WS, Simpson JA, Campbell L, Grich J. Adult attachment and the transition to parenthood. J Pers Soc Psychol 2001; 81(3): 421-35. [http://dx.doi.org/10.1037/0022-3514.81.3.421] [PMID: 11554644] |
| [36] | Hock E, Schirtzinger MB, Lutz MB, Widaman K. Maternal depressive symptomatology over the transition to parenthood: Assessing the influence of marital satisfaction and marital sex role traditionalism. J Fam Psychol 1995; 9(1): 79-88. [http://dx.doi.org/10.1037/0893-3200.9.1.79] |
| [37] | Rubin R. Maternal identity and the maternal experience 1984. [http://dx.doi.org/10.1097/00000446-198412000-00030] |
| [38] | Simpson JA, Rholes WS, Campbell L, Tran S, Wilson CL. Adult attachment, the transition to parenthood, and depressive symptoms. J Pers Soc Psychol 2003; 84(6): 1172-87. |
| [39] | Lazarus RS, Folkman S. Stress, appraisal, and coping 1984. |
| [40] | Snyder CR, Ford CE, Eds. Coping with negative life events: Clinical and social psychological perspectives 1987. [http://dx.doi.org/10.1007/978-1-4757-9865-4] |
| [41] | Beutler LE, Moos RH, Lane G. Coping, treatment planning, and treatment outcome: discussion. J Clin Psychol 2003; 59(10): 1151-67. [http://dx.doi.org/10.1002/jclp.10216] [PMID: 12968279] |
| [42] | Moos RH, Holahan CJ. Dispositional and contextual perspectives on coping: toward an integrative framework. J Clin Psychol 2003; 59(12): 1387-403. [http://dx.doi.org/10.1002/jclp.10229] [PMID: 14618606] |
| [43] | O'Brien TB, DeLongis A. The interactional context of problem-, emotion-, and relationship-focused coping: The role of the big five personality factors. J Pers 1996; 64(4): 775-813. |
| [44] | Vollrath M, Torgersen S, Alnæs R. Personality as long-term predictor of coping. Pers Individ Dif 1995; 18(1): 117-25. [http://dx.doi.org/10.1016/0191-8869(94)00110-E] |
| [45] | McCrae RR. Situational determinants of coping responses: Loss, threat, and challenge. J Pers Soc Psychol 1984; 46(4): 919-28. [http://dx.doi.org/10.1037/0022-3514.46.4.919] [PMID: 6737200] |
| [46] | Shikai N, Nagata T, Kitamura T. Do people cope with situations as they say? Relationship between perceived coping style and actual coping response. Psychiatry Clin Neurosci 2014; 68(2): 154-9. [http://dx.doi.org/10.1111/pcn.12094] [PMID: 24118236] |
| [47] | Arizmendi TG, Affonso DD. Stressful events related to pregnancy and postpartum. J Psychosom Res 1987; 31(6): 743-56. [http://dx.doi.org/10.1016/0022-3999(87)90023-7] [PMID: 3430433] |
| [48] | Ohashi Y, Takegata M, Haruna M, Kitamura T, Takauma F, Tada K. Association of specific negative life events with depression severity one month after childbirth in community-dwelling mothers. Int J Nurs Health Sci 2015; 2(2): 13-20. |
| [49] | Kendler KS, Kessler RC, Heath AC, Neale MC, Eaves LJ. Coping: A genetic epidemiological investigation. Psychol Med 1991; 21(2): 337-46. [http://dx.doi.org/10.1017/S0033291700020444] [PMID: 1876639] |
| [50] | Folkman S, Lazarus RS. If it changes it must be a process: Study of emotion and coping during three stages of a college examination. J Pers Soc Psychol 1985; 48(1): 150-70. [http://dx.doi.org/10.1037/0022-3514.48.1.150] [PMID: 2980281] |
| [51] | Burton LJ, Mazerolle SM. Survey instrument validity Part I: Principles of survey instrument development and validity in athletic training education research. Athletic Training Education J 2011; 6(1): 27-35. |
| [52] | Bentler PM. Comparative fit indexes in structural models. Psychol Bull 1990; 107(2): 238-46. [http://dx.doi.org/10.1037/0033-2909.107.2.238] [PMID: 2320703] |
| [53] | Schermelleh-Engel K, Moosbrugger H, Müller H. Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods Psychol Res Online 2003; 8(2): 23-74. |
| [54] | Akaike H. Factor analysis and AIC. Psychometrika 1987; 52(3): 317-32. [http://dx.doi.org/10.1007/BF02294359] |
| [55] | Chen FF, Hayes A, Carver CS, Laurenceau JP, Zhang Z. Modeling general and specific variance in multifaceted constructs: A comparison of the bifactor model to other approaches. J Pers 2012; 80(1): 219-51. [http://dx.doi.org/10.1111/j.1467-6494.2011.00739.x] [PMID: 2209 2195] |
| [56] | Cucina J, Byle K. The bifactor model fits better than the higher-order model in more than 90% of comparisons for mental abilities test batteries. J Intelligence 2017; 5(3): 27. [http://dx.doi.org/10.3390/jintelligence5030027] |
| [57] | Gignac GE. Higher-order models versus direct hierarchical models: G as superordinate or breadth factor? Psychol Sci Q 2008; 50(1): 21-43. |
| [58] | Reise SP, Morizot J, Hays RD. The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Qual Life Res 2007; 16(Suppl. 1): 19-31. [http://dx.doi.org/10.1007/s11136-007-9183-7] [PMID: 17479357] |
| [59] | Klein RB. Principles and practice of structural equation modelling 3rd ed. 2011. |
| [60] | Cunningham NK, Brown PM, Page AC. Does the Edinburgh Postnatal Depression Scale measure the same constructs across time? Arch Women Ment Health 2015; 18(6): 793-804. [http://dx.doi.org/10.1007/s00737-014-0485-9] [PMID: 25510935] |
| [61] | Reichenheim ME, Moraes CL, Oliveira AS, Lobato G. Revisiting the dimensional structure of the Edinburgh Postnatal Depression Scale (EPDS): Empirical evidence for a general factor. BMC Med Res Methodol 2011; 11: 93. [http://dx.doi.org/10.1186/1471-2288-11-93] [PMID: 21689442] |
| [62] | Nolvi S, Karlsson L, Bridgett DJ, Pajulo M, Tolvanen M, Karlsson H. Maternal postnatal psychiatric symptoms and infant temperament affect early mother-infant bonding. Infant Behav Dev 2016; 43: 13-23. [http://dx.doi.org/10.1016/j.infbeh.2016.03.003] [PMID: 27054496] |
| [63] | Petzoldt J, Wittchen HU, Einsle F, Martini J. Maternal anxiety versus depressive disorders: specific relations to infants’ crying, feeding and sleeping problems. Child Care Health Dev 2016; 42(2): 231-45. [http://dx.doi.org/10.1111/cch.12292] [PMID: 26490836] |
| [64] | Tikotzky L. Postpartum maternal sleep, maternal depressive symptoms and self-perceived mother-infant emotional relationship. Behav Sleep Med 2016; 14(1): 5-22. [http://dx.doi.org/10.1080/15402002.2014.940111] [PMID: 25127316] |
| [65] | Nolen-Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. J Abnorm Psychol 2000; 109(3): 504-11. [http://dx.doi.org/10.1037/0021-843X.109.3.504] [PMID: 11016119] |
| [66] | Nolen-Hoeksema S, Davis CG. “Thanks for sharing that”: Ruminators and their social support networks. J Pers Soc Psychol 1999; 77(4): 801-14. [http://dx.doi.org/10.1037/0022-3514.77.4.801] [PMID: 10531672] |
| [67] | Nolen-Hoeksema S, Morrow J, Fredrickson BL. Response styles and the duration of episodes of depressed mood. J Abnorm Psychol 1993; 102(1): 20-8. [http://dx.doi.org/10.1037/0021-843X.102.1.20] [PMID: 8436695] |
| [68] | Nolen-Hoeksema S, Parker LE, Larson J. Ruminative coping with depressed mood following loss. J Pers Soc Psychol 1994; 67(1): 92-104. [http://dx.doi.org/10.1037/0022-3514.67.1.92] [PMID: 8046585] |
| [69] | Terry DJ, Mayocchi L, Hynes GJ. Depressive symptomatology in new mothers: A stress and coping perspective. J Abnorm Psychol 1996; 105(2): 220-31. [http://dx.doi.org/10.1037/0021-843X.105.2.220] [PMID: 8723003] |
| [70] | Endler NS, Parker JD. Multidimensional assessment of coping: A critical evaluation. J Pers Soc Psychol 1990; 58(5): 844-54. [http://dx.doi.org/10.1037/0022-3514.58.5.844] [PMID: 2348372] |
| [71] | Scott KD, Klaus PH, Klaus MH. The obstetrical and postpartum benefits of continuous support during childbirth. J Womens Health Gend Based Med 1999; 8(10): 1257-64. [http://dx.doi.org/10.1089/jwh.1.1999.8.1257] [PMID: 10643833] |
| [72] | Thomas MP, Ammann G, Brazier E, Noyes P, Maybank A. Doula services within a healthy start program: Increasing access for an underserved population. Matern Child Health J 2017; 21(Suppl. 1): 59-64. [http://dx.doi.org/10.1007/s10995-017-2402-0] [PMID: 29198051] |
| [73] | Hammen C. Stress generation in depression: Reflections on origins, research, and future directions. J Clin Psychol 2006; 62(9): 1065-82. [http://dx.doi.org/10.1002/jclp.20293] [PMID: 16810666] |
| [74] | Harkness KL, Lumley MN, Truss AE. Stress generation in adolescent depression: The moderating role of child abuse and neglect. J Abnorm Child Psychol 2008; 36(3): 421-32. [http://dx.doi.org/10.1007/s10802-007-9188-2] [PMID: 18092192] |
| [75] | Wichers M, Maes HH, Jacobs N, Derom C, Thiery E, Kendler KS. Disentangling the causal inter-relationship between negative life events and depressive symptoms in women: A longitudinal twin study. Psychol Med 2012; 42(9): 1801-14. [http://dx.doi.org/10.1017/S003329171100300X] [PMID: 22273464] |
| [76] | Jomeen J, Martin CR. Replicability and stability of the multidimensional model of the Edinburgh Postnatal Depression Scale in late pregnancy. J Psychiatr Ment Health Nurs 2007; 14(3): 319-24. [http://dx.doi.org/10.1111/j.1365-2850.2007.01084.x] [PMID: 1743 0456] |
| [77] | Phillips J, Charles M, Sharpe L, Matthey S. Validation of the subscales of the Edinburgh Postnatal Depression Scale in a sample of women with unsettled infants. J Affect Disord 2009; 118(1-3): 101-12. [http://dx.doi.org/10.1016/j.jad.2009.02.004] [PMID: 19275960] |
| [78] | Vivilaki VG, Dafermos V, Kogevinas M, Bitsios P, Lionis C. The Edinburgh Postnatal Depression Scale: Translation and validation for a Greek sample. BMC Public Health 2009; 9: 329. [http://dx.doi.org/10.1186/1471-2458-9-329] |
| [79] | Lau Y, Wang Y, Yin L, Chan KS, Guo X. Validation of the Mainland Chinese version of the Edinburgh Postnatal Depression Scale in Chengdu mothers. Int J Nurs Stud 2010; 47(9): 1139-51. [http://dx.doi.org/10.1016/j.ijnurstu.2010.02.005] |
| [80] | King PA. Replicability of structural models of the Edinburgh Postnatal Depression Scale (EPDS) in a community sample of postpartum African American women with low socioeconomic status. Arch Women Ment Health 2012; 15(2): 77-86. [http://dx.doi.org/10.1007/s00737-012-0260-8] [PMID: 22297555] |
| [81] | Hartley CM, Barroso N, Rey Y, Pettit JW, Bagner DM. Factor structure and psychometric properties of english and spanish versions of the edinburgh postnatal depression scale among Hispanic women in a primary care setting. J Clin Psychol 2014; 70(12): 1240-50. [http://dx.doi.org/10.1002/jclp.22101] [PMID: 24807217] |
| [82] | Töreki A, Andó B, Dudas RB, et al. Validation of the Edinburgh Postnatal Depression Scale as a screening tool for postpartum depression in a clinical sample in Hungary. Midwifery 2014; 30(8): 911-8. [http://dx.doi.org/10.1016/j.midw.2014.02.008] [PMID: 24742635] |
| [83] | Zhong Q, Gelaye B, Rondon M, et al. Sánchez SE, García PJ, Sánchez E, Comparative performance of patient health questionnaire-9 and Edinburgh Postnatal Depression Scale for screening antepartum depression. J Affect Disord 2014; 162: 1-7. [http://dx.doi.org/10.1016/j.jad.2014.03.028] [PMID: 24766996] |
| [84] | Odalovic M, Tadic I, Lakic D, Nordeng H, Lupattelli A, Tasic L. Translation and factor analysis of structural models of Edinburgh Postnatal Depression Scale in Serbian pregnant and postpartum women - Web-based study. Women Birth 2015; 28(3): e31-5. [http://dx.doi.org/10.1016/j.wombi.2015.01.014] [PMID: 25744940] |
| [85] | Gollan JK, Wisniewski SR, Luther JF. Generating an efficient version of the Edinburgh Postnatal Depression Scale in an urban obstetrical population. J Affect Disord 2016; 208: 615-20. |
| [86] | Albuquerque MR, Corrêa H, Couto TC, Santos W, Romano-Silva MA, Santos LM. A proposal for a new Brazilian six-item version of the Edinburgh Postnatal Depression Scale. Trends Psychiatry Psychother 2017; 39(1): 29-33. [http://dx.doi.org/10.1590/2237-6089-2016-0056] [PMID: 28403320] |
| [86] | Coates R, Ayers S, de Visser R. Factor structure of the Edinburgh Postnatal Depression Scale in a population-based sample. Psychol Assess 2017; 29(8): 1016-27. [http://dx.doi.org/10.1037/pas0000397] [PMID: 27736124] |
| [88] | Kozinszky Z, Töreki A, Hompoth EA, Dudas RB, Németh G. A more rational, theory-driven approach to analysing the factor structure of the Edinburgh Postnatal Depression Scale. Psychiatry Res 2017; 250: 234-43. [http://dx.doi.org/10.1016/j.psychres.2017.01.059] [PMID: 28167438] |
| [89] | Kubota C, Inada T, Nakamura Y, et al. Stable factor structure of the Edinburgh Postnatal Depression Scale during the whole peripartum period: Results from a Japanese prospective cohort study. Sci Rep 2018; 8(1): 17659. [http://dx.doi.org/10.1038/s41598-018-36101-z] [PMID: 30518774] |